By Cassidy Miller and Louisa Weindruch
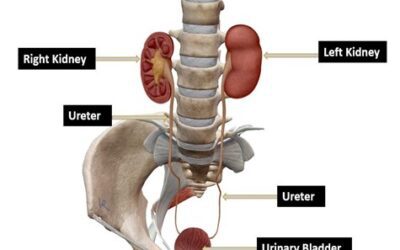
Over the last several years, access to ultrasound has increased dramatically, making point-of-care ultrasound (POCUS) a diagnostic standard across many medical specialties. It is cost effective, non-invasive, and becoming more and more portable. Physicians can now take ultrasound where it previously was unavailable, such as in rural areas, ambulances, and foreign countries for medical missions.
Despite its expanded use and applicability, many medical schools remain behind in developing and implementing ultrasound education. Due to its growing importance, we believe students should gain exposure to POCUS as early in their medical education as possible.
Point-of-care ultrasound is essential to incorporate into medical education to ensure that students are familiar with the technique, troubleshooting, and identification of both normal and abnormal anatomy. Like clinical communication or differential diagnoses, ultrasound is a skill that improves when students are given the opportunity to practice it early on.
There are many different ways POCUS can be implemented in medical schools. The University of North Texas Health Science Center Texas College of Osteopathic Medicine (TCOM) has successfully integrated ultrasound into years one and two with the help of student teaching assistants. Currently, TCOM students have exposure to ultrasound during first-year physical exams and second-year simulation lab courses. These activities are monitored by ultrasound-trained faculty but primarily carried out by the teaching assistants. The teaching assistants are year-two students who have undergone additional training and proven their skills in a graded OSCE-type assessment.

During a recent survey, we found that peer teaching assistants were the preferred method for teaching among students. This model has several benefits for both the student learners and teaching assistants. It allows students to be comfortable learning with their peers, with less fear of making mistakes or asking for help. It also gives the teaching assistants valuable teaching experience, which will inevitably be part of their medical careers in the future.
One question that remains in POCUS education is how to quantify student ability. UNT HSC is hoping to accomplish this through our newly developed micro-credentialing program. The program is a two-day course that allows students, residents, and practicing physicians to earn a certification in a specific area of point-of-care ultrasound. It’s separated into three parts—the first is the pre-work, which includes several online SonoSim modules on POCUS applications, techniques, and image acquisition. The second part is the in-person workshop where participants practice ultrasound on standardized patients and identify abnormal images. Lastly, participants are allowed to check out the Butterfly probes and must obtain several images on their own outside of the course. Ultrasound faculty then grade these images on a standardized rubric to evaluate student ability and retention of information.
Overall, point-of-care ultrasound is a vital diagnostic tool that helps clinicians streamline treatments and improve patient care. Like many aspects of medicine, students need adequate opportunities to practice before encountering POCUS in the hospital or clinic. UNT HSC has accomplished this by creating a sustainable model to help train the next generation of ultrasound users. Based on our experience, we believe peer-to-peer teaching can be an invaluable tool for programs looking to jump-start their ultrasound education.
Validate your POCUS skills with the full POCUS Certifications.
About the Authors
 Cassidy Miller is third year student at the Texas College of Osteopathic Medicine at the University of North Texas Health Science Center. Cassidy is a Senior Teaching Assistant for ultrasound curriculum and participates in several point-of-care ultrasound research projects and microcredentialling programs. She hopes to pursue a career in Family Medicine, and continue to develop her ultrasound skills.
Cassidy Miller is third year student at the Texas College of Osteopathic Medicine at the University of North Texas Health Science Center. Cassidy is a Senior Teaching Assistant for ultrasound curriculum and participates in several point-of-care ultrasound research projects and microcredentialling programs. She hopes to pursue a career in Family Medicine, and continue to develop her ultrasound skills.
 Louisa Weindruch is a third-year medical student at Texas College of Osteopathic Medicine in Fort Worth, Texas. In addition to being involved in TCOM’s Microcredential Program, she is active in ultrasound-related research and enjoys mentoring younger students as an ultrasound teaching assistant. She is interested in pursuing Emergency Medicine.
Louisa Weindruch is a third-year medical student at Texas College of Osteopathic Medicine in Fort Worth, Texas. In addition to being involved in TCOM’s Microcredential Program, she is active in ultrasound-related research and enjoys mentoring younger students as an ultrasound teaching assistant. She is interested in pursuing Emergency Medicine.