By Victor Rao MBBS, DMRD, RDMS – Abdomen, Ob/Gyn (APCA)
Introduction
Deep vein thrombosis (DVT) is a medical condition in which a thrombus develops in a deep vein, usually in the leg and/or thigh. It can also form in the pelvic/iliac veins or even upper extremities. The thrombus in the iliac veins may also extend into the IVC. Iliofemoral deep vein thrombosis is present in approximately 25% of cases. DVT can be life-threatening if the thrombus breaks loose and eventually reaches pulmonary circulation. It can travel to the blood vessels of the lung, becoming potentially fatal if it is large enough to obstruct major blood supply to the left and right lungs. This happens when a large thrombus gets obstructed in the pulmonary artery, where it divides into the left and right pulmonary arteries. This type of embolus is known as a saddle embolus and can result in sudden death in approximately 25% of individuals.
DVT is often underdiagnosed and can affect individuals of any age group. It is a preventable medical condition and POCUS can potentially alter the patient’s outcome by early diagnosis and intervention. Early diagnosis and treatment can prevent morbidity and mortality in patients. According to the Centers for Disease Control and Prevention, up to 900,000 patients are affected by this condition resulting in 60,000 to 100,000 deaths in the U.S. annually. Unfortunately, 10-30% of the individuals will die within a month of diagnosis.
In 33% of patients with a DVT they will have a recurrence within 10 years. Even though some patients may be successfully treated, 33% to 50% of those may still have residual swelling, discoloration, scaling, ulcers, and pain in the affected limb.
Common Signs and Symptoms
A small DVT or PE could also be asymptomatic. Some common signs and symptoms of a clinically significant pulmonary embolism may include the following.
- Difficulty breathing (dyspnea)
- Tachycardia
- Chest pain
- Hemoptysis
- Hypotension
- Lightheadedness
- Fainting
Role of Ultrasound as a Diagnostic Tool
Even though venography is considered the gold standard for the diagnosis of DVT, ultrasound is an excellent noninvasive modality to diagnose DVT in the upper and lower extremities. It is relatively inexpensive and more accessible with the introduction of multiple point-of-care ultrasound (POCUS) devices in the market. These devices use high-frequency ultrasound waves to create images of the blood vessels and surrounding tissue. During an ultrasound examination for DVT assessment, acoustic coupling gel is applied to the skin, and an ultrasound transducer is used to identify the deep veins of the lower extremities.
The POCUS DVT assessment is an important and easy POCUS skill to learn. Every clinician should be able to learn to effectively diagnose a case of DVT by undergoing a short training course which must include hands-on training on standardized patients and real patients with DVT. It is recommended to perform a 3-zone compression test using B-mode ultrasound. Always examine both lower extremities. Even though the patient may present with redness and swelling in one limb, there have been situations where the DVT was found in the opposite lower extremity. Bilateral ultrasound assessment is highly recommended.
Ultrasound can help diagnose clots in the deep veins, including those in the leg, thigh, and pelvis. It can also be used to evaluate blood flow using color Doppler and spectral Doppler. The method, however, has some limitations. It is not always 100% accurate. In some cases, the images produced by ultrasound may be difficult to obtain or interpret. Overall, DVT assessment using POCUS is destined to make a significant difference in the mortality and morbidity rates associated with DVT through early detection and timely treatment. Be aware that the blood clot may or may not be visible on B-mode ultrasound. The B-mode compression test is the gold standard and should be mastered by all clinicians involved in patient care.
The external, internal, and common iliac veins may be difficult to image using B-mode ultrasound. In very thin individuals you may not be able to image the above-mentioned veins. Adequate compression test may not even be possible. The thrombus may or may not be visible using B-mode imaging. Factors such as overlying bowel gas causing dirty shadow may obscure the veins. Body habitus may also create an imaging challenge. While imaging the common femoral veins you can perform a spectral Doppler assessment of the venous flow in the common femoral vein by aligning the transducer along the mid long axis of the common femoral vein. If you are unable to definitively diagnose or rule out iliac vein thrombosis and there is a strong suspicion, then contrast enhanced CT scan or venography should be considered.
Features of Blood Clot on B-mode ultrasound
B-mode ultrasound is recommended while performing the compression test for DVT assessment. However, other ultrasound modes, such as color Doppler and spectral Doppler may also be used in addition to the B-mode compression test. Since we cannot rely on the B-mode image alone the compression test must be performed when examining the deep veins in the extremities. A thrombus can appear anechoic (black) or may appear hypoechoic or even hyperechoic. In some patients, there may be an echogenic artifact that may seem like a thrombus in the lumen of the deep vein. Therefore, B-mode imaging without compression test is not dependable unless we see a clear thrombus. Even in those situations, it is recommended to perform a compression test to document noncompressible deep vein. You may also use color Doppler to show a filling defect in the region of the lumen with the thrombus.
Anatomy of Iliac Veins
The common femoral vein continues as the external iliac vein on either side after passing under the inguinal ligaments. See Figure 1 below.
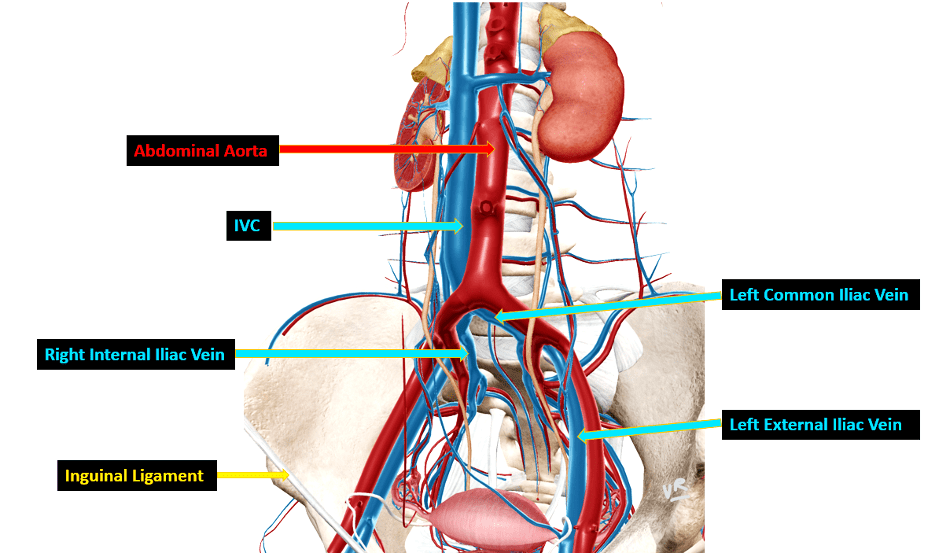
Figure 1. Diagrammatic representation of the left and right external iliac veins joining the left and right internal iliac veins respectively to form the left and right common iliac veins. The left and right common iliac veins join to form the inferior vena cava (IVC). Please note that all vessels have not been labeled.
Role of B-mode Ultrasound Imaging to Diagnose Iliac Vein Thrombosis
In some patients the iliac vein can be seen on transabdominal ultrasound. When the vein is visible on ultrasound, you can assess it using B-mode and color Doppler. See Figure 2 below showing an echogenic thrombus in the iliac vein extending into the IVC. Do note that the thrombus can also be anechoic.
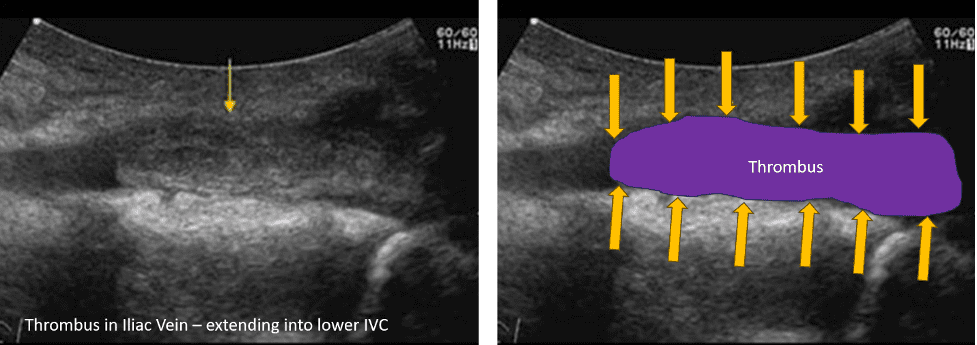
Figure 2. The image on the left shows a large echogenic thrombus in the external and common Iliac vein extending into the lower IVC. The image on the right shows the thrombus highlighted. Image on the left courtesy of UltrasoundCases.info owned by SonoSkills. The image on the right was modified from the original image to highlight the thrombus.
Role of Spectral Doppler in assessment of the External and Common Iliac Vein for a Possible Thrombus
In an unobstructed external iliac vein or common iliac vein situation, there is phasic variation observed with normal respiration during Doppler flow assessment in the corresponding common femoral vein. You can ask the patient to take deep breaths to enhance the phasicity effect. Make sure the patient is breathing actively. See Figure 3 below showing normal phasic variation in venous flow during respiration.
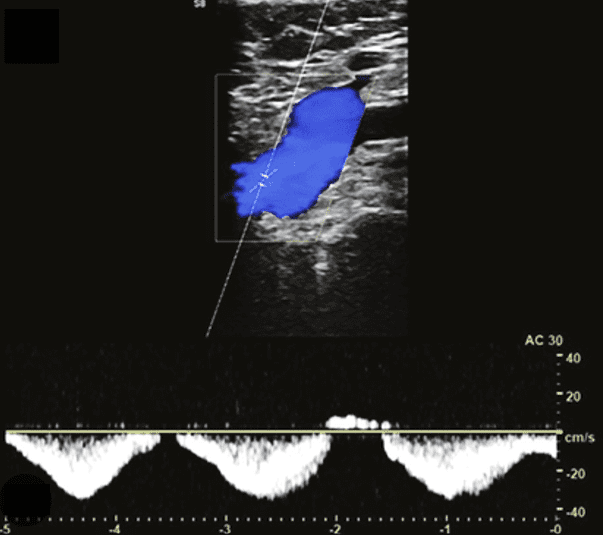
Figure 3. Normal phasic venous flow in the external iliac vein. Image courtesy of ResearchGate.
If the patient has a continuous or monophasic waveform in the left or the right common femoral vein, then it suggests high possibility of a thrombus on the corresponding side. If the monophasic waveform is observed bilaterally in the common femoral veins, then it suggests either a thrombus on both sides or in the IVC. Note that the flow could be monophasic if there is compression of the corresponding vein or an obstruction to flow in the IVC. See Figure 4 showing comparison of normal versus abnormal flow in the common femoral vein.
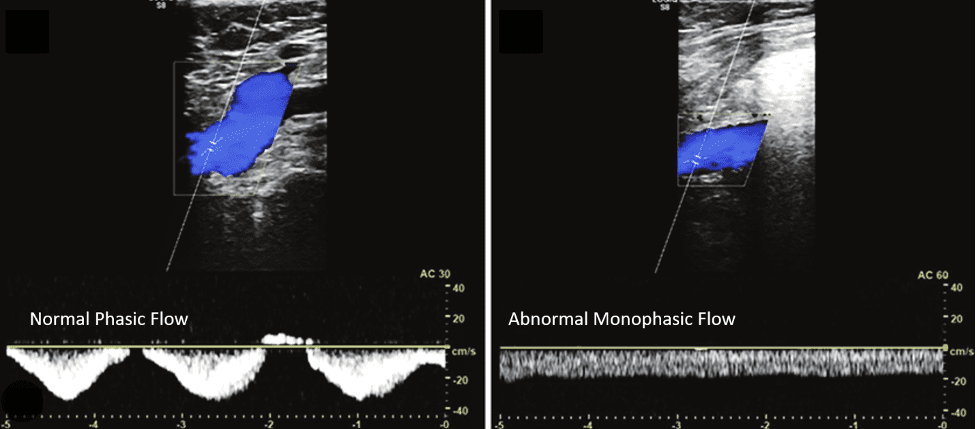
Figure 4. Normal phasic venous flow on the left and abnormal monophasic venous flow on the right on Spectral Doppler tracing of the flow in the common femoral vein. The monophasic venous flow suggests the possibility of either a thrombus in the external or common iliac vein or even the IVC. It could either be due to a thrombus or even an external compression due to a mass or an anatomical variation causing compression of the vein. Image courtesy of ResearchGate.
Final Thoughts
In conclusion, iliac vein thrombosis is best assessed by performing a spectral Doppler assessment of the venous flow in both common femoral veins. If normal phasic venous flow is seen then it is unlikely to be obstructed due to a thrombus in the corresponding external iliac vein, common iliac vein or even the IVC. You may also try to image the iliac veins using transabdominal B-mode imaging. Contrast enhanced CT scan can also be recommended to confirm suspected diagnosis. D-Dimer test should also be performed in addition to other tests. Venography may also be considered in some cases.
References
https://www.pocus101.com/dvt-ultrasound-made-easy-step-by-step-guide/
https://radiopaedia.org/articles/iliofemoral-deep-vein-thrombosis-1?lang=us