Opportunity gap. Food gap. Healthcare gap. These terms are often used to figuratively illustrate a literal need within a community. Responses to such “gaps” vary greatly—some may point and talk while others may build a bridge. The Health Wagon is the latter—an organization that builds bridges and tirelessly works to fill in complex healthcare gaps for marginalized communities.
About the Health Wagon
On a recent FOCUS on POCUS™ podcast episode, we met up with Dr. Teresa Owens-Tyson, a family nurse practitioner and President & CEO of The Health Wagon, a nonprofit free health clinic based in Wise, Virginia.
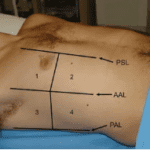
Serving Virginia’s Central Appalachian Mountain region since 1980, The Health Wagon employs a multimodal approach, serving patients at one of two stationary clinics, three mobile clinics, or through telehealth services. The Health Wagon’s patients are some of the most impoverished residents in this region. They are either uninsured or underinsured.1 Seventy percent of their patients work multiple jobs and still make less than $20,000 a year.2
During this episode, Dr. Owens-Tyson shared a few additional startling insights about the people from the Central Appalachia location: People from this region have higher mortality and morbidity rates for common ailments like heart disease, chronic obstructive pulmonary disease (COPD), and diabetes, for example, than people from other Virginia regions. Mental health illnesses and substance abuse disorders are comparatively more prevalent as well. The life expectancy of those from this southwestern community is 20 years less than their counterparts on Virginia’s Eastern Shore. As Virginia is home to several of the wealthiest counties in the nation, Dr. Owens-Tyson continues to draw attention to the stark contrast of those living without access to healthcare only a few hours away.
For their diligent efforts and accomplishments, Dr. Teresa Owens-Tyson and The Health Wagon have earned numerous awards and recognitions. Dr. Owens-Tyson has also been featured on countless national and international platforms. From interviews with 60 minutes, Nightline, and The Washington Post, to name a few, to multiple presentations before the United Nations and the World Health Organization, Dr. Owens-Tyson engages the world on healthcare access disparities and how to address them collaboratively.
Dr. Owens-Tysons has reached out to regional and state politicians to help spread the word about the dire healthcare needs in this region. Her efforts made a difference. As politicians became more aware, eventually Medicaid coverage for medical and dental expenses, respectively, was expanded in Virginia.
The Health Wagon is a leader in many ways. As a mobile health clinic beginning 40 years ago out of the back of a Volkswagen Beetle, it is the first of its kind in Virginia and possibly in the country. For over 30 years, they have been offering telehealth services—decades before COVID-19 made it a necessity for some general practitioners—and are currently the largest telehealth provider in the United States. The Health Wagon is also the first organization to become FAA-approved to use drones for medical deliveries. They are also known to have the largest medical outreaches in the United States.
Dr. Owens-Tyson makes it clear that their efforts and accomplishments would not be possible without volunteers, donations, and partnerships with medical professionals, organizations, businesses, and universities. Because of this support, The Health Wagon offers a myriad of free services, including, but not limited to, general and some specialty medical care, ultrasound services, x-rays, and, of late, COVID-19 related services.
Services Provided and POCUS
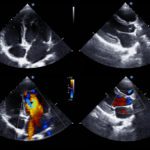
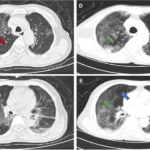
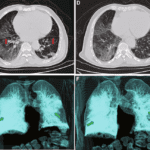
When regional hospital emergency rooms were overwhelmed with COVID testing and treatment, The Health Wagon began testing and treating patients. At one time, the COVID death rate for those in Central Appalachia was four times the state average. At the time of this podcast recording, The Health Wagon clinics had over 32,000 patient encounters, administered about 2,400 vaccines, tested over 20,000 people, and given over 5,000 monoclonal antibody infusions as COVID-19 treatments. Additionally, ultrasound technology was used to view the effects of COVID on organs. Having this technology available in the stationary and mobile clinics allowed The Health Wagon to give more holistic treatment to patients with COVID.
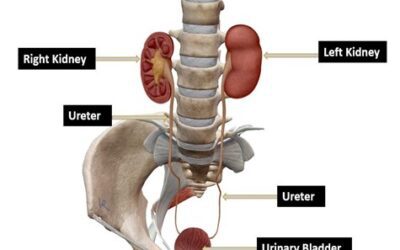
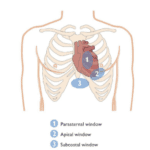
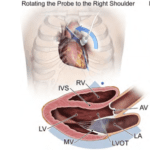
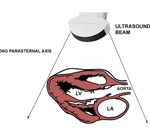
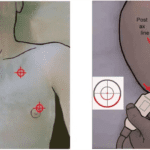
Dr. Owens-Tyson shared that point-of-care ultrasound (POCUS) technology has improved overall healthcare for this population. For example, maternal healthcare has improved, specifically for women who may experience abdominal bleeding, bloating, or even ovarian cancer. POCUS allows practitioners to view a woman’s ovaries to determine interventions. POCUS is also used to conduct transthoracic echocardiograms and check for polycystic kidney disease or chronic kidney disease. Additionally, because of volunteer doctors, scanning for various conditions such as lung masses, pneumonia, and pleural effusion are also conducted. POCUS has been great for imaging done at the mobile clinics and for bedside care in the stationary clinics. Dr. Owens-Tyson believes every technician should be taught POCUS as part of their formal medical and nursing school training. It should be as common as a stethoscope.
We at Point-of-Care Ultrasound Certification Academy™ could not agree more. Review our various training and certification offerings. If you’re interested in learning more about The Health Wagon, please visit their website or call them at 276-328-8850.
References