Victor Rao MBBS, DMRD, RDMS (APCA)
Point-of-care ultrasound (POCUS) can be used to evaluate patients with possible urinary system related complaints. These includes:
- flank or abdominal pain
- short or long standing back pain
- hematuria
- lower abdominal distension
- recurrent urinary tract infection
- dysuria
- oliguria
- nocturia
- urinary incontinence
The advantage of ultrasound is that you can image the urinary system and diagnose common pathologies such as calculi, mass, and hydronephrosis. You can easily determine bladder volume as well as post-void bladder volume to see if the patient has any significant amount of residual urine in the bladder. In most patients, the kidneys and the bladder can be efficiently imaged with ultrasound. Note that the ureters are not visualized using ultrasound unless dilated.
The ultrasound scan can be performed without any bowel preparation if needed. Being able to do so is valuable when a patient displays renal colic symptoms. The transducer of choice is a low frequency curvilinear or convex transducer with an approximate frequency range of 1.5 to 5.0 MHz. If a curvilinear or convex transducer is not available, the next best option is a phased array low frequency transducer.
Some single probe devices can also be used by selecting the correct preset. If evaluating possible calculi, be sure to scan in low lighting conditions. Also, disable the cross beam or spatial compounding feature on the ultrasound device if this option is available. It may make the stone or the associated acoustic shadowing less noticeable. The scan should be performed initially with the patient in the supine position. The patient can drink water or clear non-carbonated liquid before the exam to adequately fill the bladder.
A critical question to answer in patients experiencing pain in the flank or undergoing other related symptoms is, “Is the cause truly an obstruction to the flow of urine?” If there is an obstruction to the flow of urine from the renal pelvicalyceal system down the ureter, then ultrasound imaging should show the presence of hydronephrosis and/or hydroureter on the affected side. Both sides should be evaluated.
There are two schools of thought to grade the degree of hydronephrosis. My personal favorite is to grade the degree of hydronephrosis as mild, moderate, or severe hydronephrosis. In mild hydronephrosis, there is fullness seen in the renal pelvis only. Since urine without any debris suspended in it appears anechoic or black, the image will present an anechoic space in the renal pelvis. Make sure not to confuse this with a renal peripelvic cyst, which may look similar. You will be able to see the separation of the cyst with the renal structures and appreciate the thin wall of the renal cyst. Peripelvic cysts could also be symptomatic if they are large in diameter.
In moderate hydronephrosis, the renal pelvicalyceal system is dilated, and there is a ballooning of the minor calyces with no significant thinning of the renal parenchyma. There is evidence of significant renal parenchymal thinning with gross dilatation of the pelvicalyceal system in severe hydronephrosis. It could even appear as one large cystic structure with no evidence of renal parenchyma in extreme cases.
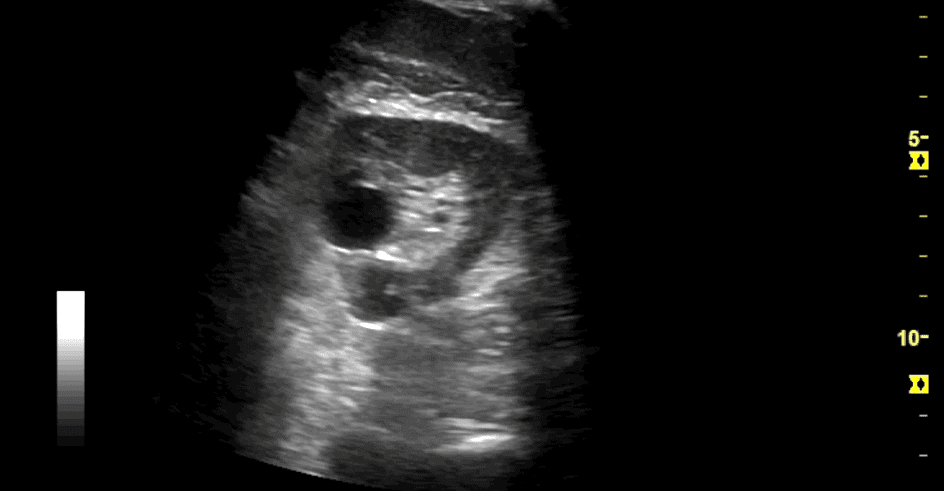
Figure showing a small renal cyst in the region of the renal pelvis.
An alternate grading system is to use the grade 0 to 4 method.
- Grade 0 is normal with no dilatation of the major or minor calyces and apposed calyceal walls.
- Grade 1 is dilatation of the renal pelvis with no dilatation of the calyces and no damage to the renal parenchyma.
- Grade 2 is similar to Grade 1 with mild dilatation of the calyces. The shape of the calyces is maintained.
- Grade 3 is when there is moderate dilatation of the pelvicalyceal system and outward ballooning of the calyces. There is minimal to no damage to the renal parenchyma.
- Grade 4 is gross dilatation of the pelvicalyceal system with evidence of damage to the renal parenchyma. In this case, the renal cortex is significantly thinner or completely flattened out.
Grade 4 is likened to severe hydronephrosis. Grade 3 is similar to moderate, while Grades 1 and 2 are considered mild hydronephrosis. Be aware that mild hydronephrosis can be viewed with a full bladder, advanced pregnancy, multiple pregnancies, or even a pelvic or abdominal mass.
Severe hydronephrosis needs to be diagnosed and treated urgently as the renal tissue has undergone significant damage. The renal tissue may be destroyed if left untreated. In some cases, moderate hydronephrosis may eventually progress to severe hydronephrosis. Here is one common scenario found in elderly male patients experiencing renal failure symptoms. After evaluation, an enlarged prostate is often found to be the culprit causing urinary retention due to urinary outflow obstruction and bilateral severe hydronephrosis.
With the proliferation of POCUS use, these cases may be diagnosed at a much earlier stage. We expect a drop in the incidence of severe hydronephrosis because of advanced benign prostatic hyperplasia. Severe hydronephrosis due to urinary outflow obstruction should never happen. The hope is, with the democratization of POCUS, preventable conditions like these will become a thing of the past.
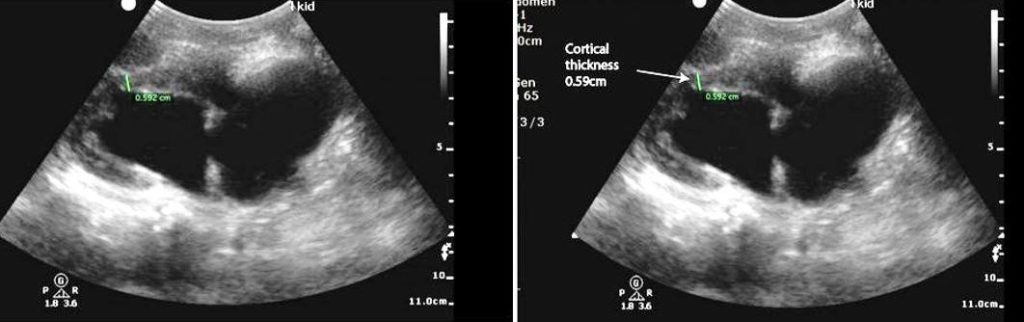
Figure (Courtesy Critical Care Sonography) showing an example of a kidney with severe hydronephrosis. Observe that the pelvicalyceal system is grossly dilated. The renal parenchymal thickness is only 0.59 cm in the image on the right. Normal renal parenchymal thickness is approximately 1.5 cm in adults. The reduction in parenchymal/cortical thickness suggests long standing severe hydronephrosis with damage to the renal parenchyma. This condition should have been diagnosed at an earlier stage when it was mild to moderate hydronephrosis. The hope is that POCUS will make this possible.
_____
Want to learn more about the impact POCUS is having on patient care? Visit our education and training resources page for more in-depth insights. Also, check out the POCUS Renal Certificate here.
























