Written by Victor V. Rao, MBBS, DMRD, RDMS
Aortic diseases and specifically abdominal aortic aneurysms (AAAs) have plagued humanity for thousands of years. The word “aneurysm” derives from two words, “aneurysma” in Greek means widening and “racemus” in Latin, meaning cluster or a bunch.
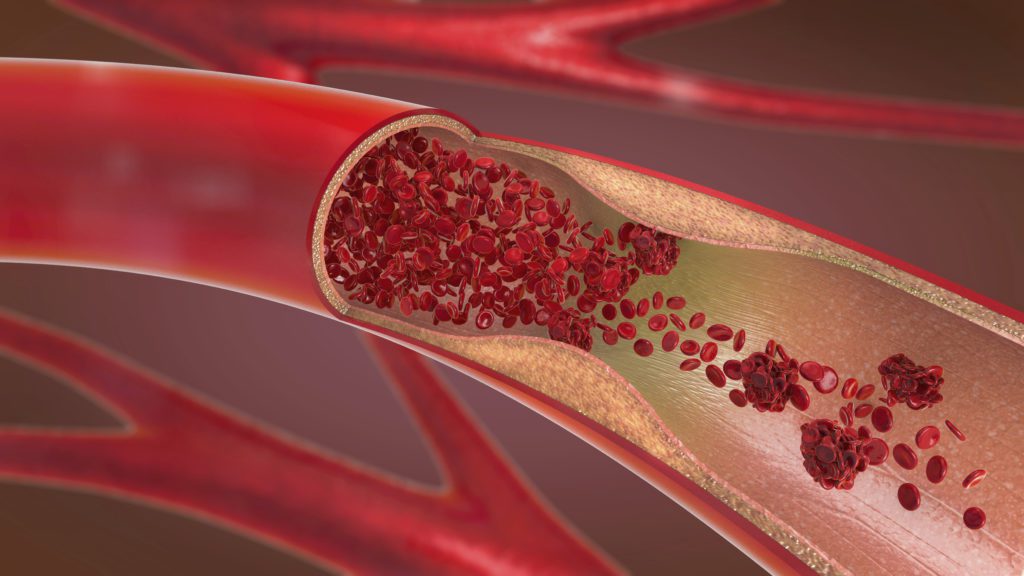
An aneurysm is simply a dilatation of the arterial wall. It is very similar to the bulging of the radiator hose in a car. If not diagnosed and replaced, it will eventually lead to a rupture of the hose, resulting in coolant leaking out.
The tension of the wall of any tube carrying fluid is directly proportional to the diameter of the tube. As the diameter increases, so will the tension of the wall of the aorta in the affected segment. The width of the pipe will continue to expand and with time, will eventually rupture.
This condition documented in Ancient Egyptian literature, mentions patients suffering from aortic aneurysms with only the ability to offer compassion to them since no treatment options were available. It wasn’t until the recent development of vascular surgical procedures during the Second World War that we see a prescription provided for abdominal aortic aneurysms.
It is ironic that though wars are devastating and cause immense human suffering, it also pushes physicians, scientists, and other professionals to the edge. This force leads to the development of new technology and medical procedures, transforming the treatment options available to the patient population. The result is a minimization of human suffering.
The experience of the surgeons treating vascular injuries on the battlefield led to attempts to repair small aortic aneurysms once they returned to their routine practice. When small aneurysm repair surgical techniques were perfected, and experience gained, the surgeons got emboldened and attempted to repair large aortic aneurysms. Further advancement occurred with the introduction of noninvasive endovascular aneurysm repair (EVAR) procedures. A treatment that significantly reduced post-procedure mortality.
At the time of the Gulf War, the Defense Advanced Research Projects Agency (DARPA) announced a grand challenge for ultrasound manufacturers to design a portable and rugged ultrasound device for the battlefield. ATL won the award, and that led to the genesis of Sonosite. Living up to the challenge, Sonosite, a rugged and transportable ultrasound machine, had its commercial market release in 1998.

The early adopters were emergency medicine physicians. Over the years, point-of-care ultrasound (POCUS) developed, and medical schools began introducing it into their medical education curriculum. Soon it became popular with physicians from other specialties, including those involved in primary care and acute care.
This phenomenon led to the detection of symptomatic and asymptomatic patients with silent abdominal aortic aneurysms in the primary care and emergency room settings. Also, other pathologies and pathophysiological states could be diagnosed in atypical medical settings. The result, timely intervention, when indicated and thus a significant lowering of AAA related deaths over the past couple of decades.
One of those interventions is screening for AAA. The United States Preventive Services Task Force (USPSTF) released an update on abdominal aortic aneurysm screening in June 2014. Men between 65-75 years old who have ever smoked are at higher risk, and according to the latest recommendations, they should undergo a one-time screening for AAA. Males who have never smoked in the same age group with other risk factors or a history suggesting a risk should consider selective screening. Included are recommendations for women as well — view the USPSTF’s final recommendation statement for full details.
Keep in mind that these are recommendations and are only applicable to routine screenings to rule out the possibility of an AAA. If a patient is symptomatic or there is suspicion of an AAA, then screening should be conducted.
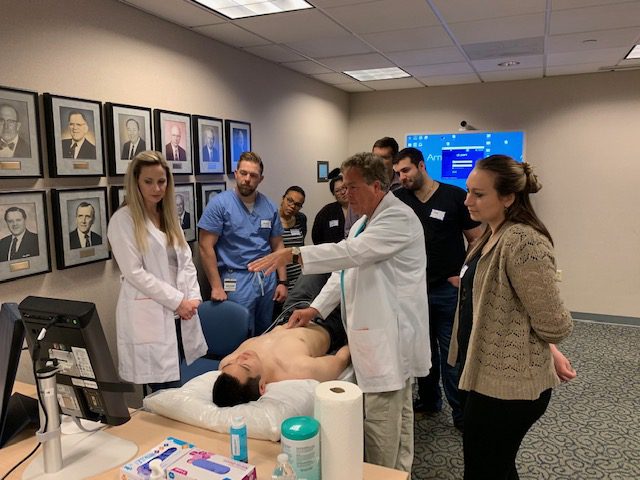
As more medical and PA schools, physicians, and other healthcare workers master POCUS and introduce it into their patient care, it is expected that the death rate due to an AAA rupture should decrease. Take caution to learn the procedure well and obtain correct measurements. Whenever in doubt, do not hesitate to refer the patient to radiology for an AAA screening.
If an AAA is diagnosed, the patient should be referred to a vascular surgeon or specialist for treatment planning and or serial follow up ultrasound exams.
For full details on the USPSTF guidelines, please visit their website.
For recommended AAA screening exam procedure guidelines, please visit the American Institute of Ultrasound in Medicine’s website.
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.





















