By Megan Lukas, RDMS
In New York City, our Emergency Department (ED) treats a diverse population of patients with a large variety of symptoms. We employ point of care ultrasound (POCUS) frequently to improve the speed and quality of their care.
The case
We recently saw a 62-year-old male presenting with shortness of breath for the past five days. His shortness of breath was acutely worsening the morning of arrival, he also was experiencing chest pressure. Due to being short of breath, he was in respiratory distress and unable to give a full medical history. He was tachypneic, hypoxic, had borderline low blood pressure, and was also found to have an elevated D-Dimer. With the information that the team had so far there were a few questions being asked:
- Does this patient have a Pulmonary Embolism?
- Is he septic?
- Is there a cardiac cause, such as congestive heart failure or acute coronary syndrome?
Given the severity of his symptoms, the team needed to initiate the proper care as quickly as possible. It would be a while before lab or radiology studies were available, so what could be done in the meantime? POCUS was the next step for the team to answer more diagnostic questions.
Why POCUS?
Point of care ultrasound is not only quick and available at the patient’s bedside, but there is no radiation exposure associated with ultrasound like there would be with an x-ray or CT scan. POCUS has become the standard of care for clinicians in Emergency Medicine and is able to provide a large amount of information for common presentations seen within the department. POCUS allows clinicians to alter their management and directly impact patient care quickly by answering focused questions based on the images that they are obtaining. When it comes to cardiac POCUS exams, there a few questions that are explored each time:
- Is there cardiac activity present?
- Is there a pericardial effusion?
- What is the global contractility?
Using four standard cardiac views, you will be able to answer these questions.
Performing basic cardiac POCUS
For a cardiac POCUS exam there are four views commonly obtained. Each view reveals a different piece of the puzzle, and they all complement each other in bringing a three-dimensional picture to life. The first view is the parasternal long axis (PSLA). When obtaining the PSLA, your probe will be placed in the third or fourth intercostal rib space, to the left of the sternum, with the probe marker pointed towards your patient’s right shoulder. In the PSLA the mitral valve, aortic valve, and apex of the heart are the three structures that should be visualized simultaneously in order to correctly assess contractility. If the probe is not orientated correctly, the assessment of contractility may be altered. The descending aorta is also visualized in the PSLA. If there is fluid seen while obtaining this view, the descending aorta acts as a landmark to help distinguish pericardial versus pleural effusion. If the fluid is seen superior to the descending aorta, that would be a pericardial effusion, whereas if the fluid is seen inferior to the descending aorta that would be a pleural effusion.
By rotating your probe marker essentially 90 degrees, towards your patient’s left shoulder you will reveal the next heart view, the parasternal short axis (PSSA). The PSSA allows for the assessment of left ventricle contractility as well as regional wall motion abnormalities due to its circumferential view. The papillary muscles are a landmark to be used to ensure you are evaluating the left ventricle at the appropriate level of the heart. Since the right ventricle (RV) is also visualized in the PSSA, you may evaluate for an enlarged RV as well.
Once you have obtained your PSLA and PSSA, the apical 4-chamber (A4C) view will allow to you to compare the right and left ventricles as well as both atria. The A4C view is obtained at the apex of the heart (approximately the 5th intercostal space), with the probe marker facing down towards the patient’s left axilla. Like the PSSL, an enlarged RV is able to be evaluated here. Although the expected ration of RV: LV size is 0.6:1; a ratio of 1:1 is often used to indicate obvious RV dilatation. The diameter is measured at the level of the mitral and tricuspid valves. The apical 4-chamber view can be difficult to obtain on some patients due to body habitus. By turning your patient into left lateral decubitus (LLD) position, the heart will move closer to the chest wall to help ensure you’re obtaining a better image. Turning your patient to LLD could also be helpful if the PSLA or PSSA views are a challenge to obtain.
The last image that we are sure to obtain to evaluate the heart is the subcostal or subxiphoid view. The liver is used as an acoustic window, enabling all four chambers of the heart to be visualized. The liver will be seen in the most superior aspect of your screen. Your probe will be placed in subxiphoid position. Since you are using the liver as an acoustic window, you will angle your probe until it is almost flat against the abdominal wall to ensure all four chambers are visualized. Your depth will also likely need to be increased so you do not miss any space surrounding the pericardium. In this view, it is important to remember that the RV is the structure closest to your probe and will be seen most superiorly. Because you are able to evaluate around the entire pericardium, the presence of fluid around the heart can be assessed.
Back to our case
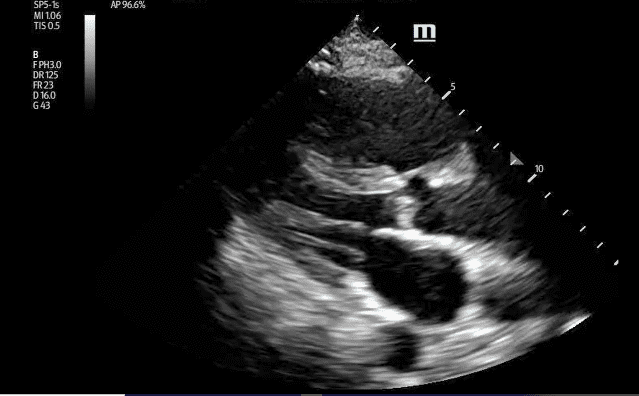
PSSL
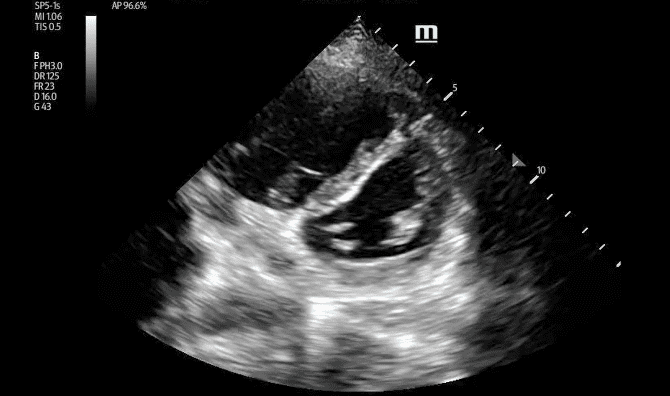
PSS
Using these four views can answer important diagnostic questions about your patient at the bedside, and a cardiac POCUS exam is exactly what the team used to ensure the best care of our patient who had presented with shortness of breath. The first view obtained by the team was the PSLA. His contractility looked good, but the RV stood out to the team. With concern for the RV size, the team moved on to the PSSA. While obtaining the PSSA, the RV also appeared dilated. When the RV becomes large enough to flatten the interventricular septal wall, it creates a “D-sign,” when there LV starts to become the shape of the letter “D”. It was apparent to the team that this was happening to their patient. The final view that the team obtained was the A4C. Since the apical four-chamber gives a full view of the heart, the team used this view to ensure the RV was enlarged. When obtaining the A4C, the septum should be oriented vertically on the screen, but due to body habitus the team was unable to have the septum straight in their images. Although there were some technical difficulties, it was obvious in this third view that the RV was enlarged. POCUS had given the team the diagnostic information that they needed to move forward with their patient’s care. The patient was then scheduled for a CT angiogram with IV contrast. The CT showed a large pulmonary embolism with CT findings of right heart strain. The patient went on to lower extremity Doppler ultrasound as well, demonstrating an occlusive right side DVT from the level of the common femoral vein to the distal femoral vein. The patient was started on Heparin, was given oxygen, and later admitted to a floor to continue anticoagulation and hemodynamic monitoring. For this patient, and so many others that are seen on a daily basis throughout the hospital, point of care ultrasound is a powerful and rapid tool that can answer critical diagnostic questions for your patients.
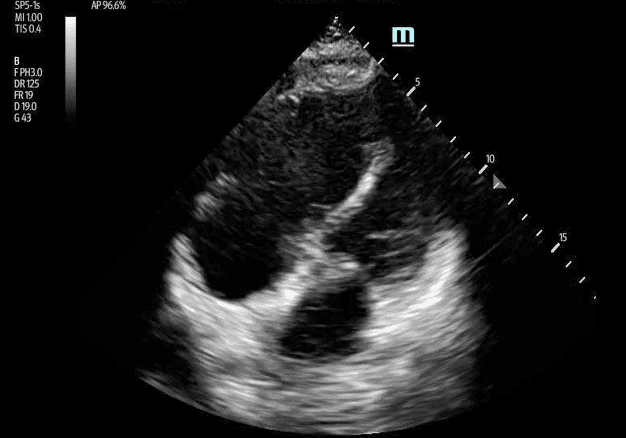
Apical 4
About the Author
Hi! My name is Megan Lukas, RDMS, and I am currently the Ultrasound Supervisor for Mount Sinai Health Systems Emergency Medicine Department in New York City. As a formally trained sonographer, I had worked in an outpatient Radiology department where I was able to grow my skills in abdominal, obstetric, vascular and musculoskeletal imaging for years before joining the team at Mount Sinai. As the Ultrasound Supervisor at Mount Sinai, I work with Ultrasound Fellows, Faculty, International Scholars, and Medical Students. My goal is to help grow their Point of Care Ultrasound (POCUS) skills and ensure proper technique through departmental educational experiences as well as on-shift education.
References
- Noble, Vicki, and Bret Nelson. Manual of Emergency and Critical Care Ultrasound. 2nd ed., Cambridge University Press, 2011.
_____
Want to learn more about the impact POCUS is having on patient care? Visit our education and training resources page for more in-depth insights. Ready to start your POCUS journey? Check out our many certificates and certifications here.





















