The State of Maternal Healthcare
The World Health Organization (WHO) defines maternal health as a woman’s health condition during pregnancy, childbirth, and postnatal care. The expectation is that every woman should experience these stages favorably and without extreme complications. The healthcare provided and available should ensure both mom and baby reach their full health and well-being potential.
Last reported by the Gates Foundation, the global maternal mortality ratio was 152 deaths per 100,000 live births in 2020, up from 151 deaths per 100,000 live births in 2019. In 2017, this amounted to 295,000 women dying during and following pregnancy and childbirth, according to the WHO. The majority of which were avoidable.
To add to these devastating numbers, The Commonwealth Fund concluded in 2020 that among 11 developed countries, the United States (U.S.) had the highest maternal mortality rate. Shortage of maternity care providers and no guaranteed access to home visits from medical providers or paid parental leave during the postpartum period were identified as contributing factors.
The state of Georgia conducted a study to look at the situation further. What research found undoubtedly pointed to inequity and inaccessibility. Top findings included:
- Varying maternal care standards
- Inequalities across population groups
- Limited maternal care financing
- Geographic hurdles to adequate medical professionals
- Affordability
The U.S. is not alone in its struggle to combat maternal health disparities. South Africa also engaged in research to unearth the barriers impacting access to proficient maternal care. The country’s maternal mortality rate is 625 deaths per 100,000 live births, exceptionally high for a middle-income country.
South Africa discovered that affordability, availability, and acceptability barriers impeded access to obstetric services. These were unequally distributed, with the most vital differences between socioeconomic groups and geographic areas. Women in rural areas face the greatest obstacles. Long travel times, higher costs associated with delivery, and lower service acceptability impede the level of care provided to moms.
An overall assessment of developing countries maintains that inaccessibility to essential health information along with the physical, economic, and sociocultural distance separating health services from the vast majority of women are significant factors plaguing maternal healthcare. Developing regions also combat the issue of limited resources. When pregnant patients do make their way to medical facilities, they battle the lack of minimal life-saving equipment and personnel scarcity or finite training.

Changing the Maternal Health Narrative
Addressing inequalities that affect health outcomes is a fundamental human right that should be in reach of every mother-to-be. Our medical community must do what’s needed to ensure all women have access to high-quality maternity care. Prevention of maternal deaths requires fundamental changes that can begin with resource allocation.
Most maternal deaths are preventable. Our medical community has the knowledge and know-how required to prevent or manage complications. To do so, skilled healthcare practitioners must attend to all births, and care should be timely and proactive. Having the ability to expediently diagnose conditions threatening the well-being of both mom and baby and being empowered to respond with treatment immediately can make the difference between life and death.
This is why we, at the Point-of-Care Ultrasound (POCUS) Certification Academy™, are so passionate about the evolution and progression of the POCUS movement. POCUS’ portability and affordability allow the modality to go where no other medical device can. It is a bedside resource that informs its user how best to tend to their patients in a matter of minutes and aids in formulating a care plan to restore and maintain perfect health.
POCUS is a low-cost imaging option that diagnoses and manages most maternal health disorders, drastically impacting lower and middle-income countries. The result—the presence of POCUS is becoming a prominent modality in healthcare facilities in urban and rural regions worldwide.
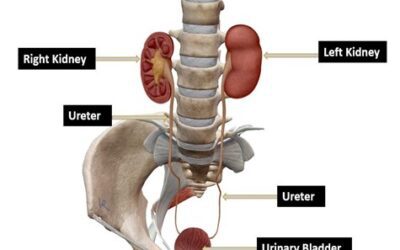
POCUS is paramount and highly useful in OBGYN emergencies. The pocket-sized device is primarily used for prognosis. A well-performed POCUS examination may detect an ectopic or extra-uterine pregnancy, a missing intrauterine gestational sac, and the presence of a tubal sac or free intraperitoneal fluid. Additional findings made via POCUS include an abnormal amount of amniotic fluid or a cervical length shortening.
Continual pregnancy assessment is critical to ensuring healthy outcomes. POCUS allows ongoing monitoring to occur in locations where resources are scarce, or medical costs create a healthcare barrier. Fetal viability, multiple pregnancy, placental position, cervical length, and amniotic fluid level are all elements of pregnancy that should be closely watched by a medical professional. Each significantly affects maternal and fetal morbidity and mortality. If they are not regularly observed, opportunities to proactively remedy life-threatening conditions are missed.
POCUS education and training are also on the uptick globally. An increase in medical schools, programs, and organizations offering formal POCUS instruction has grown substantially. At the POCUS Certification Academy alone, accessible POCUS education increased worldwide, extending to India, Australia, Canada, and Latin America. The goal is not only to get the modality into the hands of as many practitioners as possible. We also want to ensure that POCUS application is conducted in the most effective and efficient manner possible.
Becoming the Change Needed
Medicine must systematically address the access constraints facing women during pregnancy and delivery to achieve drastic declines in the maternal mortality rates and increase the standards of maternal healthcare. More must be done to respond to deterrents by improving how and where services are provided. Let’s begin with embracing and integrating the power of a hand-held device, available today yet ready to take on and change the future.