By Dr. Archan S. Patel
Lateral epicondylitis, commonly referred to as tennis elbow, is one of the most frequent causes of lateral elbow pain. This condition arises from repetitive stress on the tendons that attach to the lateral epicondyle, often due to overuse activities involving wrist extension or gripping. While clinical diagnosis is based on history and physical examination, ultrasound imaging has emerged as a useful, non-invasive diagnostic tool, offering real-time visualization of the tendons and associated structures. This article provides an in-depth guide to using point-of-care ultrasound (POCUS) for assessing lateral epicondylitis.
What is Lateral Epicondylitis?
Lateral epicondylitis is a degenerative condition affecting the extensor tendons, primarily the extensor carpi radialis brevis (ECRB). It typically occurs due to repetitive overuse, leading to microtears and subsequent degeneration and/or inflammation. Patients often present with lateral elbow pain, difficulty gripping objects, and reduced strength. While it is most common in individuals who perform repetitive motions, such as athletes or manual laborers, it can affect anyone engaging in repetitive wrist extension or gripping activities.

Ultrasound imaging offers dynamic imaging and detailed insights that clinical examination alone may not provide.
Anatomy
A thorough understanding of the lateral elbow anatomy is essential for accurate ultrasound assessment. Key structures include:
Extensor carpi radialis brevis (ECRB): The primary tendon implicated in lateral epicondylitis, originating from the lateral epicondyle. It is innervated by the radial nerve (C5-C8), and its primary actions include flexing the elbow and extending/abducting the hand.
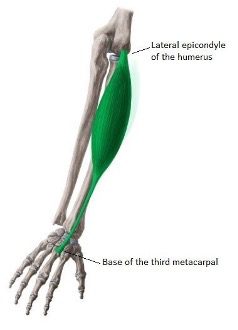
Figure 1. Extensor carpi radialis brevis (green) with origin on the lateral epicondyle of humerus and insertion on the base of the third metacarpal.
Extensor digitorum communis (EDC): Another extensor tendon often involved in the pathology. Also known as the “common digital extensor.” Its primary function is to extend the medial four digits at the metacarpophalangeal joints, and at the interphalangeal joints, in addition to extending the wrist joint.

Figure 2. Extensor digitorum communis (green) with origin on the lateral epicondyle of humerus and insertion in the extensor hoods of medial four digits.
Lateral ulnar collateral ligament (LUCL): An important stabilizer of the elbow joint for varus stress and external rotation, located adjacent to the extensor tendons.
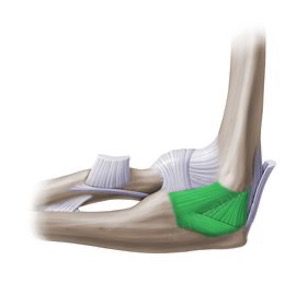
Figure 3. Lateral ulnar collateral ligament (green) with origin on the lateral epicondyle of humerus and insertion on the tubercle of the supinator crest.
Radial nerve: Runs proximally and may mimic symptoms if compressed (radial tunnel syndrome).
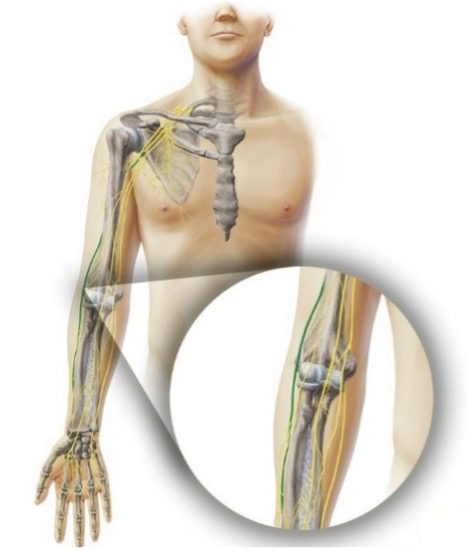
Figure 4. Radial nerve course (green) originating from the posterior cord of brachial plexus (C5-T1). It is the largest branch of the brachial plexus.
Cortical bone: The lateral epicondyle serves as the bony attachment site for the extensor tendons.
Indications for Ultrasound
POCUS is particularly valuable in the following scenarios:
- Persistent Lateral Elbow Pain: When symptoms do not resolve with initial conservative treatment.
- Suspected Tendinopathy or Tear: To identify tendinosis, partial or full-thickness tendon tears.
- Pre-Intervention Assessment: Ensuring precise localization of pathology before administering corticosteroid (CS) or platelet-rich plasma (PRP) injections or performing Ultrasound-Guided Percutaneous Tenotomy.
- Rule Out Differential Diagnoses: Conditions such as radial tunnel syndrome, and bursitis.
Patients presenting with localized tenderness over the lateral epicondyle, pain exacerbated by gripping or lifting, or reduced grip strength are ideal candidates for ultrasound evaluation.
Ultrasound Equipment and Settings
For the best results, the following settings and equipment are recommended:
- Transducer: High-frequency linear probe (10-15 MHz) for optimal visualization of superficial structures.
- Modes: Use grayscale (B-mode) for structural assessment, color Doppler and power Doppler to evaluate vascularity.
- Depth: Adjust to focus on the lateral epicondyle and surrounding tendons (approximately 1-3 cm deep).
- Gain and Focus: Optimize settings to enhance visualization of tendon fibrils and bony landmarks.
Ultrasound Technique
Patient Positioning
- Position the patient comfortably seated, with their arm resting on a flat surface.
- The elbow should be flexed at 90°, with the forearm in pronation and the hand relaxed.
Scanning Protocol
- Longitudinal View: Align the probe parallel to the long axis of the lateral epicondyle and extensor tendons. This view highlights the fibrillar structure of the tendons.

Figure 5. Patient arm and ultrasound probe position in longitudinal view.
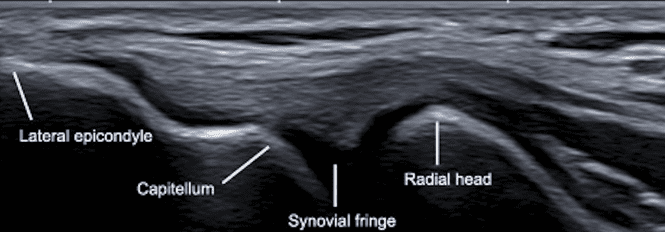
Figure 6. Ultrasound image of lateral elbow highlighting the common extensor tendon fibrillar structure in longitudinal view.
2. Transverse View: Rotate the probe 90° to obtain a cross-sectional view, evaluating tendon thickness and echotexture.

Figure 7. Patient arm and ultrasound probe position for transverse view.
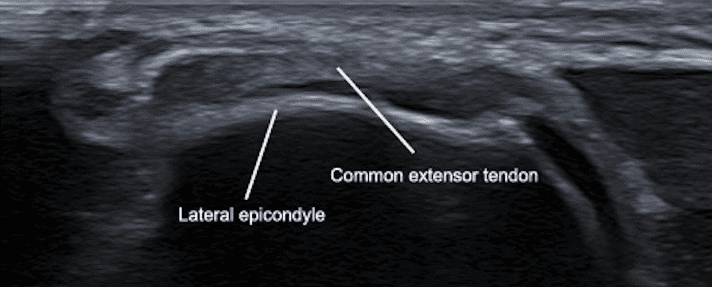
Figure 8. Ultrasound image of lateral elbow highlighting common extensor tendon thickness and texture in transverse view.
3. Distal Transverse View: Maintain the probe perpendicular to the long axis of the lateral epicondyle and extensor tendons, and move it distally to obtain a cross-sectional view, evaluating tendon thickness and echotexture.

Figure 9. Patient arm and ultrasound probe position for distal transverse view.
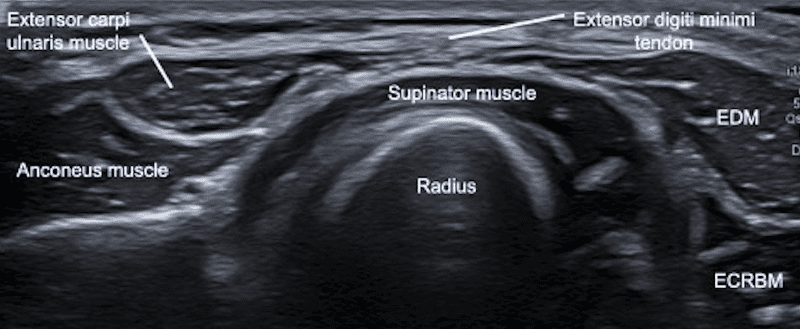
Figure 10. Ultrasound image of distal lateral elbow in transverse view (ECRBM = Extensor Carpi Radialis Brevis Muscle).
- Dynamic Assessment: Ask the patient to perform resisted wrist or finger extension during the scan to detect subtle abnormalities or pain reproduction.
- Doppler Evaluation: Use color Doppler or power Doppler to assess hypervascularity, which is often indicative of neovascularization in chronic tendinopathy.
Key Landmarks
- Lateral Epicondyle: Visualized as a hyperechoic cortical surface, serving as the bony attachment site for extensor tendons.
- Common Extensor Tendon: Appears as a fibrillar, hyperechoic structure originating from the lateral epicondyle.
- Radial Head: Evaluate for joint effusion or other abnormalities proximally.
Pathological Findings in Lateral Epicondylitis
Tendinosis
- Hypoechoic, thickened tendons with disrupted fibrillar architecture.
- Small hyperechoic calcifications may be visible, often with posterior shadowing.
Partial-Thickness Tears
- Focal hypoechoic or anechoic areas within the tendon, indicating localized disruption.
Full-Thickness Tears
- Complete discontinuity of the tendon fibers, often accompanied by retraction.
Enthesopathy
- Irregularity or erosion at the bony attachment of the tendon.
Hypervascularity
- Increased Doppler signal reflecting neovascularization associated with chronic tendinopathy.
Bursal Effusion
- Fluid accumulation in the radial or adjacent bursae, occasionally coexisting with lateral epicondylitis.
Clinical Applications
Diagnostic Utility
- Early Diagnosis: Ultrasound detects subtle tendon changes before they become clinically significant.
- Differential Diagnosis: Distinguishes lateral epicondylitis from other conditions like radial tunnel syndrome or osteoarthritis.
Interventional Guidance
- Corticosteroid Injections: Ensures precise placement into the affected area, minimizing risk to surrounding structures.
- Platelet-Rich Plasma (PRP) Therapy: Facilitates targeted delivery of PRP to promote tendon healing.
Monitoring Progress
Ultrasound is invaluable for tracking tendon healing and guiding rehabilitation programs, ensuring optimal outcomes.
Limitations and Challenges
Despite its benefits, ultrasound assessment of lateral epicondylitis has limitations:
- Operator Dependence: Requires skill and experience for accurate interpretation.

Figure 11. Improper ultrasound probe scanning technique.
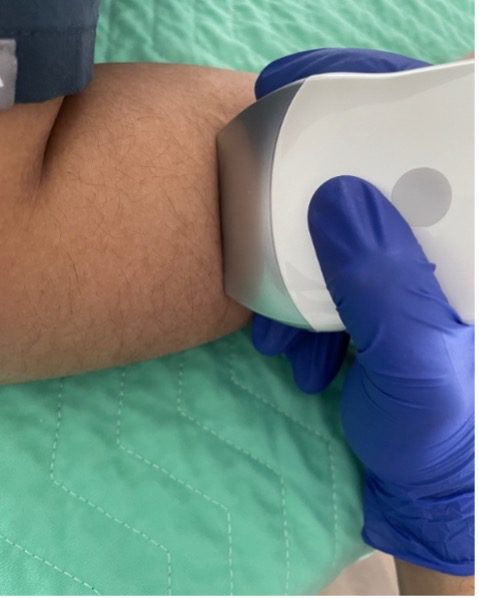
Figure 12. Proper ultrasound probe scanning technique.
- Depth Penetration: Superficial structures are well-visualized, but deeper joint pathology may require advanced imaging like MRI.
- Chronic Cases: Extensive structural damage may necessitate further diagnostic evaluation.
Enhancing Your Skills
Clinicians can refine their musculoskeletal ultrasound skills by participating in specialized MSK POCUS training programs that cover:
- Ultrasound anatomy and scanning techniques.
- Interpretation of musculoskeletal pathologies, including tendinopathy and tears.
- Hands-on training for guided interventions.
These programs empower clinicians to integrate ultrasound seamlessly into their practice, enhancing diagnostic accuracy and patient care.
Conclusion
Ultrasound is an invaluable tool for clinicians. Its ability to provide detailed, dynamic imaging enhances diagnostic accuracy and supports targeted treatment strategies, improving patient outcomes. By mastering these techniques, healthcare providers can confidently diagnose, monitor, and treat lateral epicondylitis, ensuring the highest quality of care.
For more information and resources, visit the POCUS Certification Academy and take the next step in your musculoskeletal ultrasound journey.
References
- Draghi F, Danesino GM, Gautard R, Bianchi S. Ultrasound exploration of the elbow: a user-friendly approach. Eur J Radiol. 2023;158:110896. doi:10.1016/j.ejrad.2023.110896
- Fletcher D, Sarkar M. A grounded theory of psychological resilience in Olympic champions. Psychol Sport Exerc. 2012;13(5):669-678. doi:10.1016/j.psychsport.2012.04.007
- WikiSM (Sports Medicine Wiki). Common Extensor Tendon Injection. WikiSM. Published [date unavailable]. Accessed March 9, 2025. https://wikism.org/Common_Extensor_Tendon_Injection
- Sports Medicine Review. Quick Guide to Diagnostic Ultrasound of the Elbow. SportsMedReview.com. Published [date unavailable]. Accessed March 19, 2025. https://www.sportsmedreview.com/blog/quick-guide-to-diagnostic-ultrasound-of-the-elbow/
- Rubin GD. Performing an Ultrasound-Guided Lateral Epicondyle Injection. SportsMedReview.com. Published [date unavailable]. Accessed March 24, 2025. https://www.sportsmedreview.com/blog/performing-an-ultrasound-guided-lateral-epicondyle-injection/




















