By: Victor V Rao MBBS, DMRD, RDMS- Abdomen, Ob/Gyn (APCA)
Introduction
The spleen is an intraabdominal organ and is the largest organ of the lymphatic system. The healthy adult spleen weighs approximately 200 grams and measures 12-14 cm in length. It is in the left hypochondrium (left upper quadrant) between the left hemidiaphragm superiorly and the fundus of the stomach medially. In some patients the spleen may be challenging to image in its entirety with ultrasound due to overlying bowel gas or patient body habitus. It is important to know the exact anatomical location of the spleen and the structures surrounding it to be able to visualize it successfully with ultrasound. The goal should be to direct an unobstructed ultrasound beam between the lower intercostal spaces towards the spleen along its mid long axis.
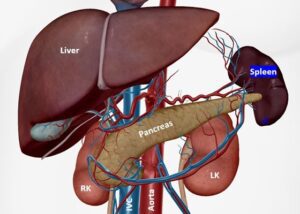
Figure 1. Observe the location of the spleen in the left hypochondrium and other important anatomical structures in the area. The stomach and colon are not shown in this image but are shown in Figure 2. Also note that the tail of the pancreas abuts against the splenic hilum.
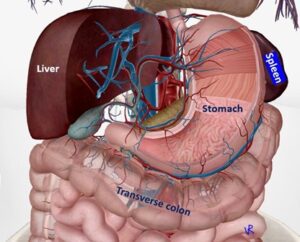
Figure 2. Note the location of the stomach and the colon to the spleen. Presence of excessive air in the stomach and or splenic flexure of colon can be a barrier to optimal imaging of the spleen.
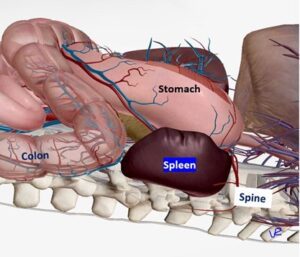
Figure 3. Side view of the spleen obtained from the left side. This helps understand why the knuckles and dorsum of the hand holding the transducer should be toughing the bed surface. Ribs are not shown in the figure to uncover the underlying organs.
Scan and Measurement Technique and Tips
Scan the patient with a low frequency transducer in the supine position with the transducer/probe marker pointing cephalad (toward the head of the patient) to obtain a longitudinal view. You will have to rotate the probe clockwise or counterclockwise to eliminate the rib acoustic shadows.
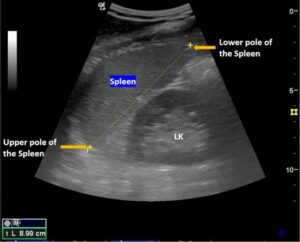
Figure 4. Mid-longitudinal view of the spleen. Measure from upper pole to the lower pole as shown. Observe that the spleen’s superior surface is convex and is right under the left hemidiaphragm. If the patient has splenic injury with hemorrhage, the blood may collect in the space between the spleen and the left hemidiaphragm. In this example there is no evidence of fluid in that space. This view was obtained using a low frequency convex/curvilinear transducer.
Adjust the depth to approximately 18-20 cm initially and once the spleen is visualized in the longitudinal axis, the depth can be adjusted to optimize the image. If the patient has an enlarged spleen, you may not be able to image the entire spleen even with maximal depth and may have to use panoramic image mode to stitch the images together to image the entire spleen. See Figure 8.
One helpful tip while scanning the spleen is to scan from the lateral chest at the level of 8-10th intercostal space and slide the transducer posteriorly with the knuckles and even the dorsal surface of your hand holding the transducer resting on or touching the patient’s bed while aiming the ultrasound beam superiorly and medially towards the spleen. You may also ask the patient to take a deep breath and hold the breath while you scan and capture an optimal image. Once an optimal mid-longitudinal view of the spleen is obtained with the superior and inferior pole of the spleen in the image, freeze the image and measure the length of the spleen as shown in Figure 4.
Splenomegaly
Splenomegaly simply means enlarged spleen. The spleen can also be evaluated by physical exam of the abdomen. The Castell sign is suggestive of splenomegaly. See reference.
Some common causes of splenomegaly are:
- Cirrhosis of the liver
- Cystic fibrosis
- Cytomegalovirus
- Infectious mononucleosis (commonly due to Epstein-Barr virus)
- Hemolytic anemia Example – thalassemia
- Hodgkin’s disease
- Leukemia
- Lymphoma
- Malaria
Below as some examples of splenomegaly cases.

Figure 5. Splenomegaly due to Hodgkin’s disease. Image courtesy of www.ultrasoundcases.info.
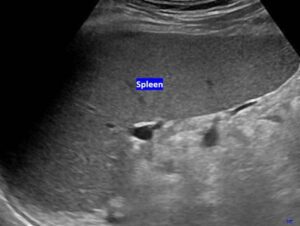
Figure 6. Splenomegaly. Spleen is enlarged due to cirrhosis. The patient also had ascites which is not obviously seen in this image. Image courtesy of www.ultrasoundcases.info.

Figure 7. Splenomegaly – malignant lymphoma. Multiple large hypoechoic lesions are seen in the spleen. Image courtesy of www.ultrasoundcases.info.
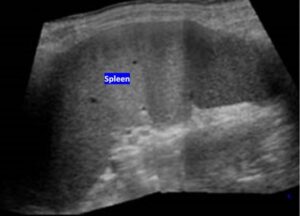
Figure 8. Splenomegaly due to chronic lymphocytic leukemia. The spleen is huge, and a special technique was used to create this image by sliding the transducer and stitching multiple images together to create a panoramic view of the spleen. Some ultrasound devices may have this function. www.ultrasoundcases.info.
Conclusion
Point-of-care ultrasound (POCUS) can be used to evaluate the spleen for various conditions, such as splenomegaly, perisplenic free fluid due to occult bleeding in trauma patients, and splenic infarction. POCUS can be considered a valuable diagnostic imaging tool in the initial evaluation of patients with suspected splenic pathology.
With a clear understanding of the anatomy and good amount of hands-on experience every POCUS user should be able to confidently image and measure the splenic length as well as look for evidence of fluid in the perisplenic space. Keep in mind that splenic injury or contusion may not be easily identifiable on ultrasound in some cases and if suspected should be referred for a CT scan of the abdomen when indicated to rule out that possibility.
References
https://stanfordmedicine25.stanford.edu/the25/spleen.html
https://radiologykey.com/spleen-scanning-protocol/
https://radiopaedia.org/articles/splenomegaly?lang=us





















