09/30/18
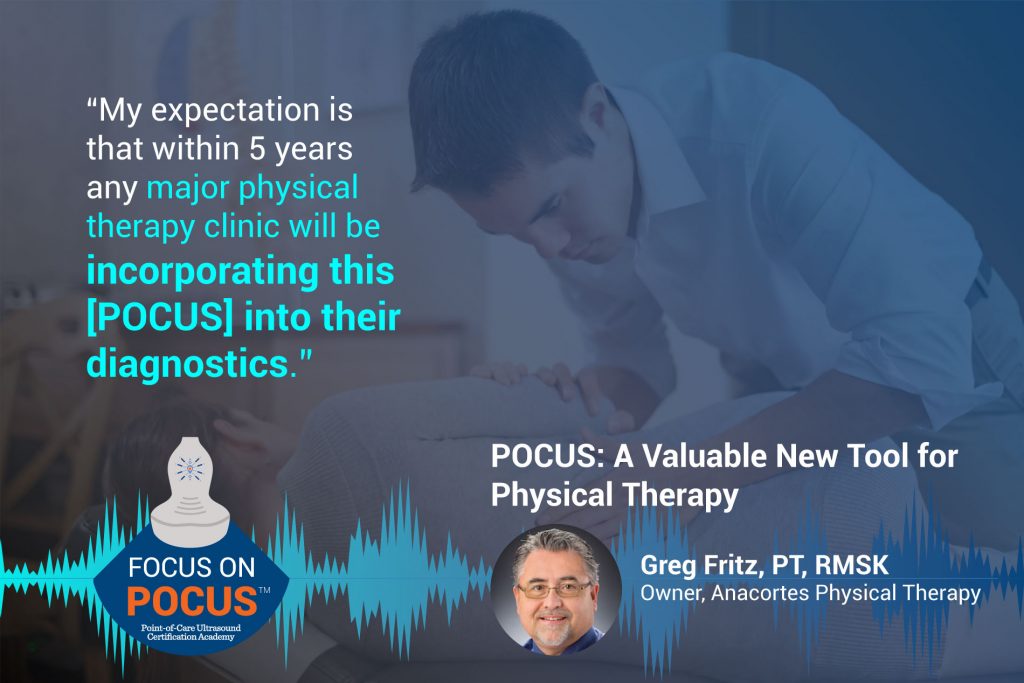 Greg Fritz was in a compulsory post pregnancy ultrasound when he saw his son’s forming bones inutero. He asked himself “Why don’t we use this to look at bones and muscles on my patients?” This started his passion/obsession for POCUS MSK. Greg was one of 3 Physical Therapists in the nation to pass the pioneer RMSK certification in 2012. Greg lectures at the university of Washington and is on the training faculty for interventional POC orthobiologics.
Greg Fritz was in a compulsory post pregnancy ultrasound when he saw his son’s forming bones inutero. He asked himself “Why don’t we use this to look at bones and muscles on my patients?” This started his passion/obsession for POCUS MSK. Greg was one of 3 Physical Therapists in the nation to pass the pioneer RMSK certification in 2012. Greg lectures at the university of Washington and is on the training faculty for interventional POC orthobiologics.
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.
Transcription:
James Day: Hello and welcome to the Point-of-Care Ultrasound Certification Academy Podcast, where we Focus on POCUS. Here we will discuss all things related to point-of-care ultrasound: The practice, the trends, and its impact on healthcare. Our program will engage thought leaders who are defining global patient care with the stethoscope of the future.
James Day: James Day here today, recording live from the Focus on POCUS studio. Today, we have Greg Fritz as our guest. Greg Fritz was in a compulsory post pregnancy ultrasound when he saw his son’s forming bones in utero. He asked himself, “Why don’t we use this to look at bones and muscles in my patients?” This started his passion, or rather obsession, for point-of-care musculoskeletal ultrasound.
James Day: Greg was one of three physical therapists in the nation to pass the Pioneer RMSK certification in 2012. Greg lectures at the University of Washington, and is on the training faculty for Interventional Point-of-Care Orthobiologics.
James Day: Hi, Greg. How are you today? How’s everything in Seattle?
Greg Fritz: I’m fine, James
James Day: Good, good. Great to have you. I think your story is one of the more interesting that we come across. So I guess to start it out here, I was gonna ask you just bluntly: How did you learn point-of-care ultrasound?
Greg Fritz: I would have to say that was trial and error. I was fortunate enough to have an uncle that was really an early adopter of ultrasound in his internal medicine practice. He was probably the second to have color doppler in the state. So I saw his passion early on, but it wasn’t until I saw my own son wiggling around that I said to myself, “Why can’t I see that?” Fortunately, my uncle had a number of older machines that finally he said to me, “Here, why don’t you just take this and see if it is of any value in your patients.” This was back probably in 2005. From there, I just grabbed the anatomy book and started looking at my kids, and then I just was amazed at what I could see. That’s my story. I am self-taught. Thanks to Netter and everyone else how writes good anatomy books and my willing children.
James Day: That’s great! So now what are you doing? I know now that you’ve evolved from that. What do you use now, machine and your scanning focus?
Greg Fritz: Yeah, I guess now from an educational standpoint there are so many different venues, and it has grown into such a big area of ultrasound musculoskeletal. I use it in my practice daily, multiple times a day for a number of pivotal decisions regarding patient care and treatment direction. So I guess, I hope, and I think that’s my answer. You can refine that if you’d like.
James Day: I was just thinking, how common is it that the physical therapists, say, I’m going to see a knee sprain using muscle skeletal ultrasound in their practice?
Greg Fritz: That’s a good question because musculoskeletal ultrasound as far as real-time or diagnostic dynamic ultrasound in the practice of physical therapy is a presently exploding area of interest. I don’t know as far as in the Seattle area there may be one or two other therapists that will use it to refine diagnoses on patients or monitor changes in inflammation. But it’s so rapidly being adopted that I would believe that any major area will have this as a part of the evaluation within two to three years. My expectation is that within five years any major physical therapy clinic will be incorporating this into their diagnostics or at least their evaluation of patient progress.
James Day: Great, great. So physical therapists, they read their own studies, right? And make calls from that?
Greg Fritz: That’s kind of an interesting question or assumption. Physical therapists have long made some conclusions based on manual tests or orthopedic tests of joints. We’ve been able to say, “Is that joint stable? Or is that joint unstable?” And there’s a number of named tests to evaluate, let’s say, the rotator cuff to see if there’s a tear. If you did five of those specific tests, you could come up with specificity or a sensitivity that would make you feel fairly confident in saying that’s a rotator cuff tear. But if a physical therapist places a scanner or probe over the supraspinatus tendon and they can see that it is intact, they’re able to say there’s not a tear in the supraspinatus tendon. So most therapists that recognize that what you see is reality will then ultimately be able to say there is or is not a tear here. Therapists have the ability to draw conclusions based on data they collect during an evaluation.
Greg Fritz: But I think the question might go on further to say: Does a therapist have the ability to generate an official document that you would expect out of like radiologists offices or medical. The reality is physical therapists presently don’t have a good route to go about billing specifically for this particular evaluation. So it is as valuable to a therapist as far as evaluation as their hands and goniometers and strength evaluation dynamometers, and we can draw conclusions from that. So yes, we can read the results of what the ultrasound shows. We’re not gonna be generating an official report for insurance to review that we’ll get compensated for. Does that make sense?
James Day: Yes, that does. The reason I ask you something like that because I know you own your own physical therapy clinics, I’m not sure, I don’t remember. We talked about it at a convention once. So I guess since you are a business owner, I was gonna ask you how it started evolving. How do you go about billing for a point-of-care ultrasound study? Is it in your state? Is it happening?
Greg Fritz: That’s a fair question. What comes up when I do presentations to my peers is that return on investment or ROI. How do I get my money back for the expense of the unit and the expense of education? There are two answers to the question. If you become an RMSK certified practitioner through the APCA if you can become an RMSK practitioner, insurances are willing to compensate you for the actual performance of the evaluation. We’re still in the process of developing the ability to actually generate and be able to have access to the CPT code for the interpretation of that. But uniquely there are plenty of radiologists that are out there that are willing to take fax with your report and make it official. So that is a billable item under that particular model.
Greg Fritz: But when I talk to my fellow therapists, it’s really a function of what brings patients in the door. The marketing potential of me actually showing a patient their tendon moving and the quantity of inflammation that’s within the fibers of their tendon, I would like to see any patient that leaves my clinic with that ability of information to process to go to any of my peers in the area and see whether they’d get by with just testing it with their hands. To me, the delineation and what it has opened up from a business growth standpoint just because I know how to use it, it’s phenomenal. So I would say from a marketing standpoint and from a credibility standpoint, it’s aces.
James Day: Wow, that’s great. I think your story is so fascinating. You’re this entrepreneur who took it upon himself to learn all aspects of point-of-care ultrasound. I guess one of the questions I was gonna ask you, maybe you have an incident or case, share a time when you used point-of-care ultrasound, and it was a standout case and made a difference in your patient care.
Greg Fritz: Yeah, that happens daily. In fact, just yesterday I had a patient that came in with a shoulder problem, and they were having numbness into their hand. As a therapist, we immediately have to say is it a rotator cuff tear, or is it a nerve root irritation at the neck? There were so many unique similarities to a nerve issue at the neck and a problem at the shoulder, the ability to simply throw a probe, scan the rotator cuff, and assure yourself and the patient that their weakness and inability to lift their arm has nothing to do with the mechanical attachment of their rotator cuff muscle, it immediately has a start to differentiate: This is of a spinal origin.
Greg Fritz: So when I have the ability to evaluate whether there’s bursitis or tendonitis, and a person is having problems at the shoulder … You know, just yesterday to be able to say, let’s focus our effort on the neck. You know, we don’t ignore the fact that most people need strength, but it allows me to put more octane into the real area of the problem, whereas I know before, a therapist would be going, should I focus 50 percent on a rotator cuff pathology or go a different route.
James Day: Wow, I find your story fascinating. I really appreciate you taking the time to be here on today’s show. I think it’s really unique that you’re calling us and you’re in a car in a parking lot next to a Starbucks. It sounds great, the audio, and we’re also giving the props out to a local Seattle business … it’s worldwide now. And it’s an honor, it’s an honor to have you on our podcast.
Greg Fritz: James, it was a pleasure. If I could just somehow get my profession to see what I see … or anybody in the musculoskeletal arena … I feel thrilled to do that. So I hope that can help everyone.
James Day: Greg, thanks a lot.
Greg Fritz: You’re welcome.
James Day: We hope you enjoyed today’s podcast: Focus on POCUS. Be sure to tune in with us next week for more interviews with thought leaders that are on the forefront of global point-of-care ultrasound.