I remember the medical school and residency season of my life. What jogs my memory most is the work, the friends, the wealth of new knowledge and above all, the anticipation of the new adventures that awaited me. As I reminisce about this period in my life, I can only describe this anticipation as a joy and an excitement of finally holding the permission slip granting me access to do the thing I love.
I couldn’t wait to take off running down the aisle of passion in pursuit of a career that with the promise of a fulfilled life. I’ve learned over the years that my path to purpose isn’t as smooth and straight forward as I perceived. Along the way to fulfillment are unexpected twist and turns I could not have seen waiting for me curbside.
This same reality hits many of us as we began to walk down the road of accomplishment. As physicians, our original intent for diving into such a challenging vocation can get lost in a sea of administration, insurance compliance, fragmented care and—let’s not mention at times—the dreaded electronic health record (EHR) systems. The flames that drove us to dedicate so much time in earning our practitioner credentials are fizzled out by all the nuances that distract us from the very reason we are here.
This dwindling ember that barely leaves us with a spark is known as burnout. Annals of Internal Medicine defines burnout as “emotional exhaustion, feelings of cynicism and detachment from work, and a low sense of personal accomplishment [1].” The complete opposition of the sentiments experienced when we take the first step on our journey to becoming a physician.
It is important to note that the effects of physician burnout are not self-impacting alone. Due to the nature of our work, burnout becomes a burden that public health must bear. If it were just you and I experiencing this lassitude and cynicism, then maybe we could pretend it doesn’t exist. However, according to an article in The Washington Post, a study reveals that half of all physicians experience some sign of burnout [2]. With 50% of us encountering symptoms of burnout, along with the expected 100,000 physician shortage by 2035—it is time to pay attention.
Dr. Gordy Johnson, hospitalist and president of the medical staff at Legacy Emanuel Medical Center in Portland, Oregon, shares with us a few side effects of physician burnout. He mentions, “The most common sign of burnout is loss of bedside manner.” The detachment from the work brought on by this condition leads us to forget the compassion required to do our jobs well. Without even realizing it, we venture away from the heart of it all.
Making increased medical mistakes is another result that seeps in, just one symptom that leads to so many others. Soon, our patients are less satisfied and malpractice cases are overwhelming banging down our doors.
Dr. Johnson warns that this ultimately can lead to depression and self-harm. The physician suicide rate is much higher than the general public’s and even exceeds that of combat veterans [3]. “We see this in our community of doctors, and that is why we, the physician community, are trying to eliminate physician burnout,” expressed Dr. Johnson.
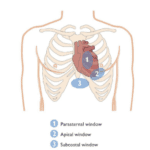
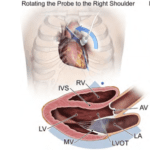
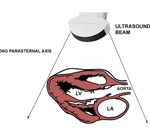
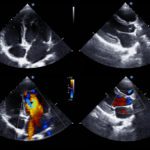
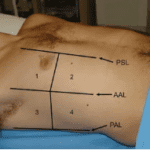
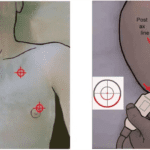
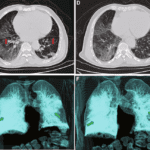
A tool used in doing so is point-of-care ultrasound (POCUS). Dr. Johnson believes there is an overarching benefit this handheld device offers. “By learning a skill such as POCUS, we get back to the bedside with our patients and enhance our interaction with them.” Patient care rises to the top once again using POCUS. It is not only how it helps us better connect with our patients in their time of need that is afresh, but POCUS also enables us to provide the level of care we initially envisioned providing. This modality helps us arrive at a diagnosis quicker, initiate procedures safer and provides us with an inside view into the anatomy of the human body we have always imagined.
That is why we began this path. We were enamored with human anatomy, fixated on correcting the disarray within and wishing for a glimpse beyond the surface. Now we have it, our dream realized.
Point-of-care ultrasound enhances the professional satisfaction of the physicians. “Professional satisfaction is working at the top of one’s license. Our professional satisfaction is everything about the job outside the wages that keeps us engaged as doctors. The relationships with patients and colleagues, the work we do, and the personal joy physicians get by helping people through difficult times is our professional satisfaction,” describes Dr. Johnson.
Even the process of learning how to use handheld ultrasound brings us back to our training days. Most of us love to learn and the challenges POCUS presents rejuvenate us, bringing on new cases that help us expand on our knowledge base.
Physicians are reinvigorated through point-of-care ultrasound. It doesn’t provide a solution for all the complexities that lead to physician burnout. Nonetheless, it is a new direction to take along our path of pursuing our passion to help others by providing the best possible healthcare to each and every patient. You can learn more about POCUS certificates and certifications for physicians here.
[1] S. Han, T. Shanafelt, C. Sinsky, K. Awad, L. Dyrbye, L. Fiscus, M. Trockel, J. Goh. Estimating Attributable Cost of Physician Burnout in the United States. Annals of Internal Medicine. https://annals.org/aim/article-abstract/2734784/estimating-attributable-cost-physician-burnout-united-states. June 4, 2019.
[2] D. Marchalik. Why are so Many Doctors Burning Out? Tons of Real and Electronic Paperwork. Washington Post. https://www.washingtonpost.com/health/why-are-so-many-doctors-burning-out-tons-of-real-and-electronic-paperwork/2019/05/31/3335ca78-346c-11e9-af5b-b51b7ff322e9_story.html?utm_term=.a75976d9304b. June 1, 2019.
[3] P. Huang. What’s Doctor Burnout Costing America? NPR. https://www.npr.org/sections/health-shots/2019/05/31/728334635/whats-doctor-burnout-costing-america. May 31, 2019.
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.