By Victor V Rao MBBS, DMRD, RDMS (APCA)
Lung ultrasound has gained popularity in recent years. The COVID-19 pandemic showed the power of Point-of-Care Ultrasound (POCUS) and lung ultrasound by enabling physicians and other healthcare workers to scan and triage hundreds of thousands of patients quickly. A recent POCUS25 survey conducted by the Point-of-Care Ultrasound Certification Academy™ ranked lung ultrasound as the top POCUS skill to learn, as identified by POCUS users worldwide.
The medical education community witnessed the role that POCUS lung played during the pandemic. The number of medical schools adopting a POCUS curriculum doubled due to the device’s life-saving impacts. We can assess the chest wall, ribs, pleura, and lungs for conditions such as:
- Subcutaneous emphysema
- Rib fractures
- Pneumothorax
- Pneumonia
- Interstitial syndrome
- Atelectasis
- Lung abscess
- Pleural effusion
- Empyema
- Lung infarction
- And many more conditions involving the lung, pleura, chest wall, and chest cavity.
Ultrasound guided procedures such as thoracentesis, chest tube insertion, and biopsies can be done safely with a much lower risk of during and post-procedure complications.
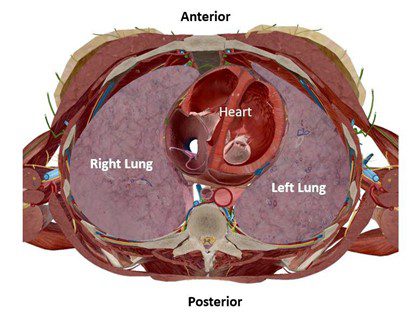
Figure 1. Cross section through mid-chest (approximately T6 level) showing the left and the right lung.
In this blog, we will briefly examine the basics of lung ultrasound and some normal lung ultrasound findings and B-lines. It is imperative to be familiar with ultrasound physics, normal lung ultrasound findings, and the limitations of ultrasound technology to execute POCUS proficiently. This would help us determine if the results are normal or abnormal and help us understand why we are visualizing certain findings.
Transducer
The transducer of choice would be a low-frequency curvilinear transducer. Some clinicians also report using a phased array transducer. You may also use a high-frequency linear transducer to assess the chest wall, pleura, or subpleural lesions. The high-frequency transducer is not ideal for imaging deeper structures or evaluating A-lines and B-lines beyond a certain depth from the skin surface.
Select the “lung” preset before scanning. B-mode imaging is useful to image the structures in the chest wall, pleura, and lungs. M-mode may be used to assess for pneumothorax in addition to B-mode. If scanning with a single probe device, select the lung preset for optimal settings. If you are using an older device, you may also choose the abdominal preset if the lung preset option is not available.
Patient Position
The patient can be scanned in the supine, lateral decubitus, or sitting upright position. An upright position may be preferred if the patient is having difficulty breathing.
Normal Lung Ultrasound Findings
The normal aerated lung ultrasound image obtained with the probe marker pointing cephalad shows a classic finding known as the “Bat sign.” The outer periosteum of the ribs represents the bat’s wings, and the pleural line between two adjacent ribs represents the bat’s body. This sign helps confirm that we are visualizing the correct space. The “Bat sign” is more helpful in obese patients to identify an intercostal space and confirm the correct placement of the ultrasound transducer because we may not be able to confirm the intercostal space by palpation alone.
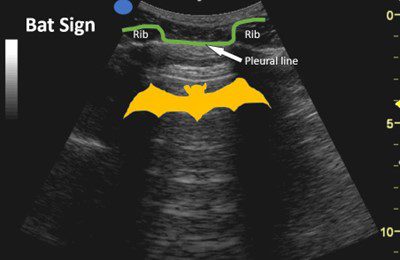
Figure 2. Bat sign.
On ultrasound we will see the chest wall, ribs with rib shadows and intercostal spaces. The normal pleural interface is seen as a hyperechoic shimmering line when the patient is breathing. On close observation we can visualize the visceral pleura sliding against the parietal pleura. The parietal pleura is attached to the inner lining of the chest wall. During inspiration and expiration, we can visualize the visceral pleura moving along with the lung surface against the parietal pleura. This is known as lung sliding. Normal aerated lung will show A-lines. A-lines are reverberation artifacts.
A-lines
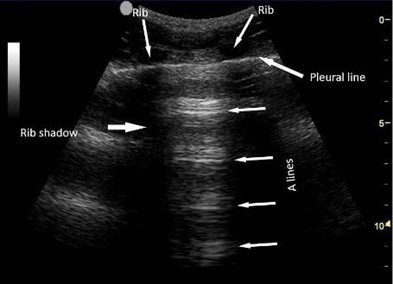
Figure 3. A-lines, pleural line, ribs, and rib shadows.
A-lines are horizontal echogenic lines running parallel to the pleural line. They are equidistant from each other, as seen in the image above. They are reverberation artifacts created when the ultrasound beam interacts with the air in the lung alveoli. It is important to remember that A-lines alone is not conclusive of a normal aerated lung. However, A-lines and normal lung sliding suggest normal aerated lung in the intercostal space during the observed time.
If the lung sliding is only observed for a short time during breathing, it may indicate the presence of lung point, which is consistent with pneumothorax. If lung sliding is absent at a level, it may suggest pneumothorax. Prominent A-lines may also be seen in asthma and chronic obstructive pulmonary disease (COPD).
B-lines
B-lines, also referred to as comet tails, are vertical artifacts that appear as echogenic lines and extend from the pleural line into the lung parenchyma. They are created by discreet short path reverberation artifacts due to interstitial edema, increased fluid, or fibrosis in the interlobular septae. They are well-defined unless they become confluent.
The B-lines tend to extend through the lung field and do not become less bright, unlike A-lines, which tend to become less echogenic with depth. They also erase or cancel out the A-lines, and it is important to note that they move with respiration. One to two B-lines may be seen in some elderly individuals in the lung bases. It is considered an abnormal finding if three or more B-lines are identified in an intercostal space.
The figure below shows the progression of findings from normal A-line profile to a B-profile and eventually consolidation in a patient with COVID-19.
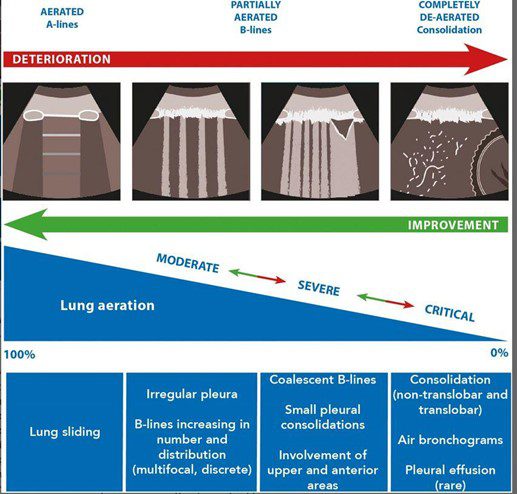
Figure 4. Lung ultrasound findings of normal, moderate, severe, and critical pleural and lung parenchyma changes in patients with COVID-19. (Courtesy wileylibraryonline.com)

Figure 5. Multiple B-lines
The decision tree below shows how to use lung ultrasound findings to evaluate a patient with acute respiratory failure. If lung sliding is seen in all lung fields bilaterally and three or more B-lines are visible in an intercostal space, it suggests pulmonary edema. The presence of lung sliding in all fields will also rule out the possibility of pneumothorax. A mixed picture with A and B lines is consistent with pneumonia. Even though lung sliding is not observed, the presence of B-lines rules out pneumothorax in the lung zone scanned. Note that B-lines can only be produced through lung tissue. Lung point is consistent with pneumothorax. Always correlate clinically, and do not hesitate to use other imaging options to come to a final diagnosis if in doubt.
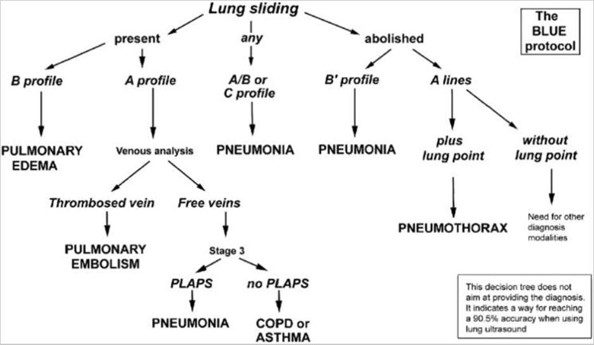
Figure 6. The BLUE Protocol. Courtesy Daniel A. Lichtenstein et al. (2008). Relevance of Lung Ultrasound in the Diagnosis of Acute Respiratory Failure. This iconic decision tree is quite helpful and uses the A-lines and B-lines in addition to some other lung ultrasound findings to determine the cause of acute respiratory failure.
Conclusion
Lung ultrasound is a relatively seamless skill to learn and should be an essential one to master for all physicians and healthcare workers. Knowing fundamental physics, recognizing A-lines and B-lines, and using the clinical decision tree can expedite clinical diagnosis. This can lead to appropriate, timely treatment and help lower the morbidity and mortality rates associated with acute respiratory failure.
References
Baker, W., Carmody, K., Hagopian, L., Husain, L., Wayman, D. (2012). Sonographic diagnosis of pneumothorax. Journal of Emergencies, Trauma, and Shock, 5(1), 76-81. https://pubmed.ncbi.nlm.nih.gov/22416161/
Hayward, S.A., Innes, S.M., Miller, A.S.C., Smith, M.J. (2020). Point-of-care lung ultrasound in patients with COVID-19 – a narrative review. Anaesthesia, 75(8), 1096-1104. https://associationofanaesthetists-publications.onlinelibrary.wiley.com/doi/10.1111/anae.15082
Lichtenstein, D., Meziere, G. (2008). Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest Journal, 134(1), 117-125. https://journal.chestnet.org/article/S0012-3692(08)60155-5/fulltext