By Khushal Choudhary, MD, Cardiology Fellow, SUNY Downstate University Hospital, Brooklyn, NY
Aortic stenosis (AS) is one of the most common valvular heart diseases, especially in the aging population. It affects roughly 2–6% of individuals over age 65 and presents with a wide range of symptoms—from none to fatigue, angina, syncope, and even sudden cardiac death.
So, how do we spot it early and manage it effectively? Point-of-care ultrasound (POCUS) is a powerful tool in the initial evaluation and monitoring of aortic stenosis, especially in symptomatic patients or those with incidental murmurs.
When Should You Suspect Aortic Stenosis
Evaluation should be considered in:
- Symptomatic patients (fatigue, chest pain, dizziness, or syncope)
- Incidental findings (like a murmur heard during routine exam)
- Individuals with a family history of valvular heart disease (Bicuspid valve)
Let us walk through a quick case scenario
A 69-year-old man with a history of hypertension, diabetes, hyperlipidemia, and prior PCI to the LAD presents with Canadian Cardiovascular Society (CCS) class III angina, worsening fatigue, and lightheadedness. Time to perform a limited POCUS echo.
What to look for on physical examination
On auscultation, aortic stenosis often presents as a harsh, crescendo-decrescendo systolic murmur best heard at the 2nd right intercostal space, radiating to the carotids. Physical examination alone is not enough, echocardiography remains the gold standard for diagnosis and grading.
POCUS Views to Evaluate the Aortic Valve
At the bedside, POCUS allows you to quickly obtain the necessary views and Doppler measurements. Here is your checklist:
1. Parasternal Long and Short Axis — At the level of the aortic valve
2. M-Mode — To assess valve motion
3. LVOT Diameter — Measured in parasternal long axis
4. Five-Chamber View — For Doppler measurements:
- LVOT VTI (using pulsed wave (PW) Doppler)
- Aortic Valve VTI (using continuous wave (CW) Doppler) *
5. Four-Chamber View — For assessing left ventricular function
*Be aware that some POCUS devices may not have CW Doppler capability.
The Science Behind It: Continuity Equation & VTI
Two key concepts help estimate the aortic valve area (AVA): the continuity equation and velocity time integral (VTI).
- The continuity equation is based on the principle that flow (volume per time) remains constant:
Flow in = Flow out
In other words, blood flowing through the LVOT should equal that through the aortic valve (assuming no major regurgitation). - VTI represents the distance blood travels during systole. It’s measured using Doppler and reflects the area under the velocity-time curve.
How to Calculate Aortic Valve Area (AVA)
Here’s a simplified step-by-step:
1. Measure LVOT diameter from the parasternal long axis view (Figure 1).
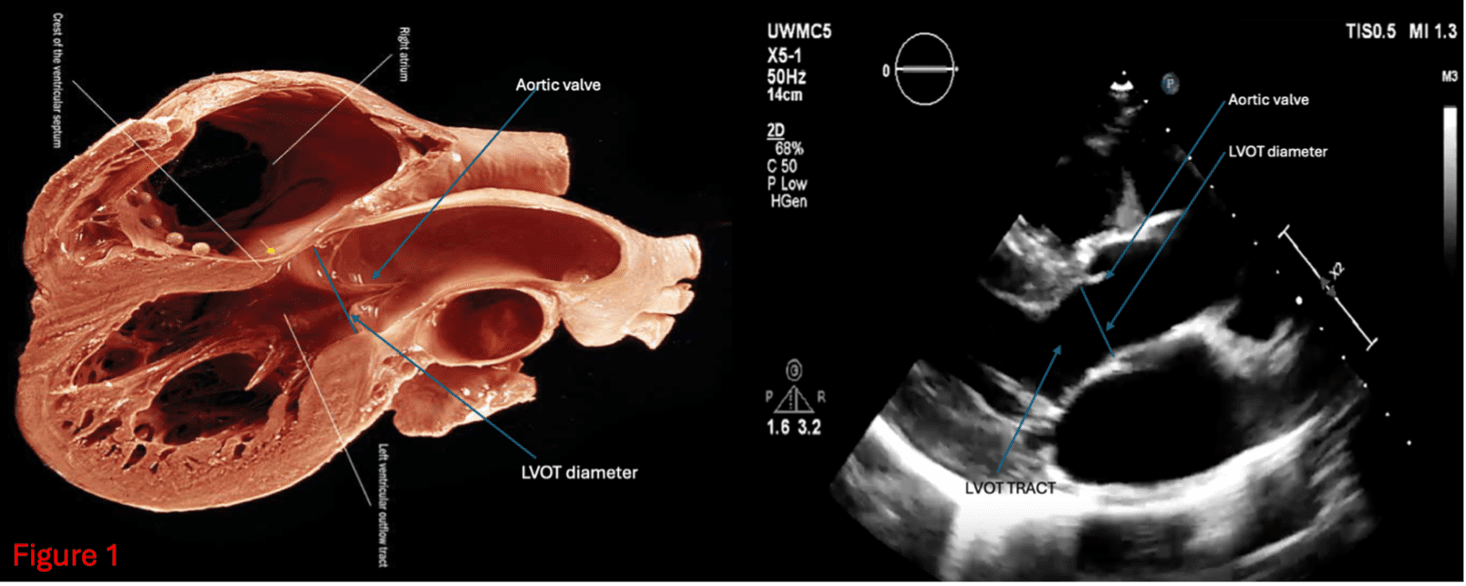
Figure 1
2. Obtain LVOT VTI using pulsed wave Doppler just proximal to the aortic valve (Figure 2)
3. Measure Aortic Valve VTI using continuous wave doppler distal to the aortic valve (Figure 3)
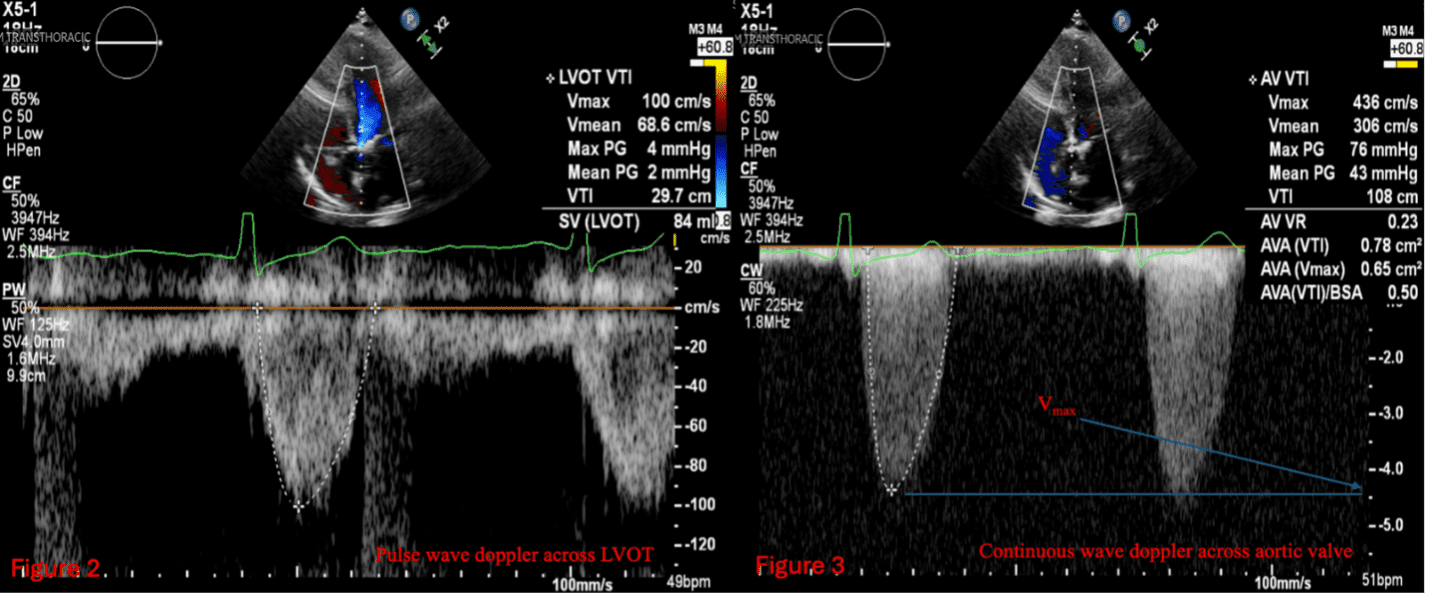
Figure 2, Figure 3
Then use the formula (Figure 4):
AVA = CSALVOT × VTILVOT / VTIaortic valve
CSA (cross-sectional area) is calculated from the LVOT diameter: CSA = π × (Diameter/2) ²
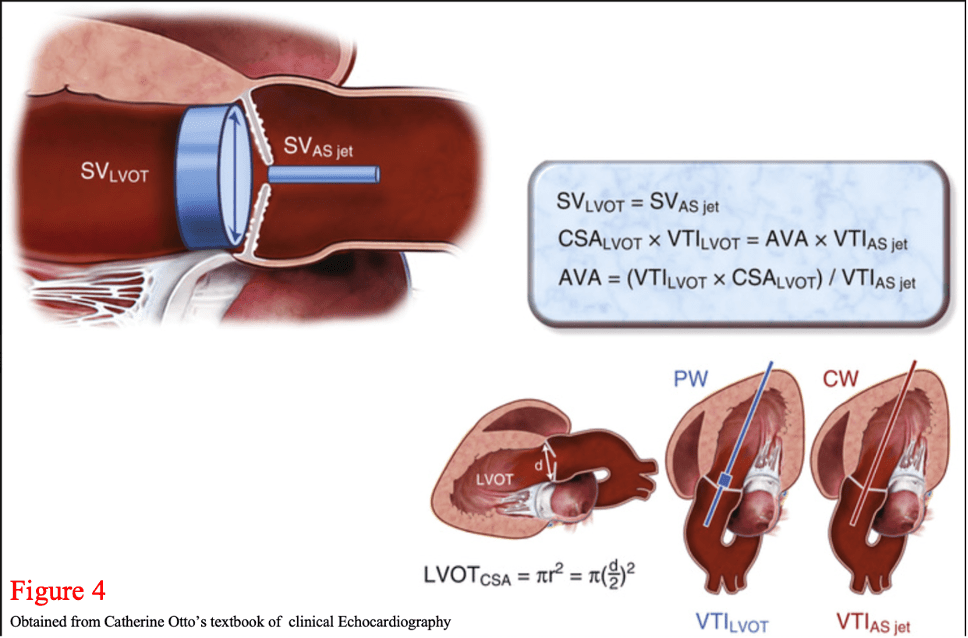
Figure 4
Grading Aortic Stenosis Severity
| Grades | Aortic Valve Area (cm2) | Jet Velocity (m/s) | Mean Gradient (mmHg) |
| Mild AS | >1.5 | 2.5-3 | <20 |
| Moderate AS | 1-1.5 | 3-4 | 20-40 |
| Severe AS | <1.0 | >4 | >40 |
Flow-Gradient Classifications
Sometimes, the severity of AS isn’t straightforward. That’s where the flow-gradient classification comes in:
| Type | Stroke Volume | Mean Gradient |
| High Flow / High Gradient | > 35 mL/m² | > 40 mmHg |
| High Flow / Low Gradient | > 35 mL/m² | < 40 mmHg |
| Low Flow / High Gradient | < 35 mL/m² | > 40 mmHg |
| Low Flow / Low Gradient (Paradoxical AS) | < 35 mL/m² | < 40 mmHg |
Approach to Aortic Stenosis Management
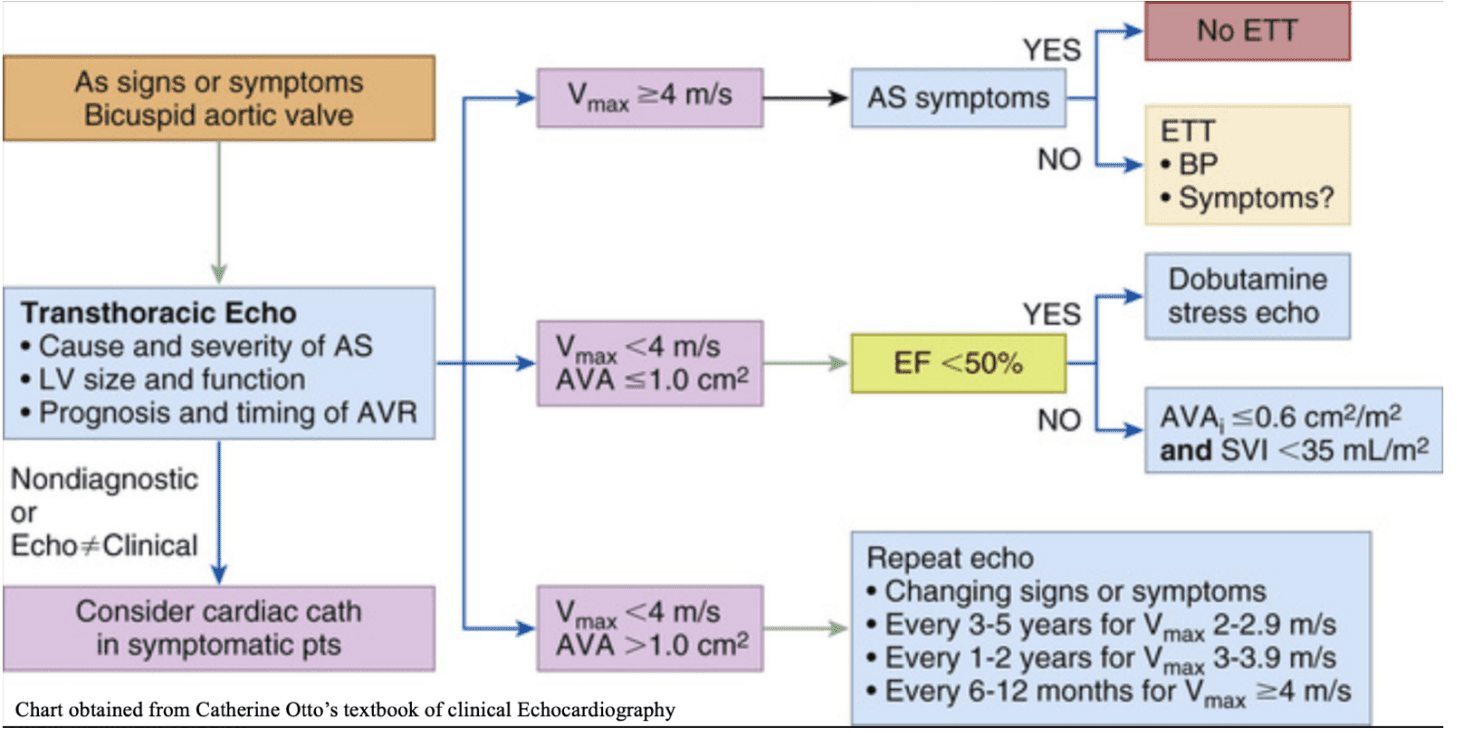
Figure 5
Final Thoughts
Bedside POCUS is an incredibly valuable skill for evaluating aortic stenosis, especially in settings where formal echocardiography is not available. Mastering these views and measurements gives you a fast, reliable way to assess severity and guide further workup or referrals.
Further Reading
- Otto, C. M. Textbook of Clinical Echocardiography, 6th Ed.
- Libby, P. et al. Braunwald’s Heart Disease, 12th Ed.




















