Victor V Rao MBBS, DMRD, RDMS
Chest ultrasound was not explored to its fullest potential for several decades, even though it was introduced into clinical practice more than 50 years ago. Radiologists had documented the use of ultrasound to diagnose:
- Pleural Effusion
- Atelectasis
- Peripheral Based Lung Abscess
- Pleural Thickening
- Pleural Mass
- Pulmonary Embolism/Infarct
- Arteriovenous Malformation
- Enlarged Lymph Nodes
- Ultrasound-guided Thoracentesis and Chest Tube Placement
The reason for slow integration was simply due to anatomy. Healthy human lungs are air-filled (except during the intrauterine phase of life). It is a well-known fact that the diagnostic ultrasound beam cannot penetrate air, making it impossible to image structures in the chest that have air in front of them. Instead, it would reflect the ultrasound beam and create imaging artifacts. The amount of air in the lung and the volume of interstitial fluid in the interstitial lung tissue can result in unique lung artifacts and patterns.
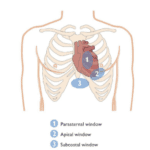
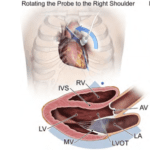
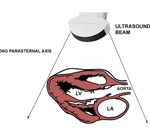
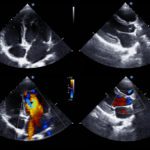
We do image the heart using ultrasound, through select intercostal spaces on the chest wall, which do not have aerated lung tissue in front of it. These areas are known as acoustic windows, and they provide an unobstructed view of the heart in most patients.
The phased array cardiac transducer with a small footprint was designed because the sonic window is only one intercostal space wide. It is specifically for echocardiography to provide ultrasound images absent of any rib shadows.
It is only recently, with the introduction of point-of-care ultrasound (POCUS), have non-traditional users of ultrasound imaging started exploring the chest with an open mind. This observation includes documenting consistent ultrasound findings and patterns in patients with clinical conditions such as pneumonia, pneumothorax, CHF, and differentiating between CHF and COPD exacerbation. POCUS users started using B-mode/2D, M-mode, color, and Power Doppler modes in the chest with the introduction of interesting and unique terminology to describe rare patterns and findings such as “Seashore sign,” “Barcode sign,” and “Jellyfish sign” to name a few.
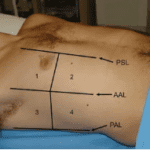
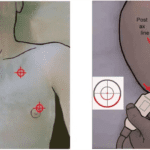
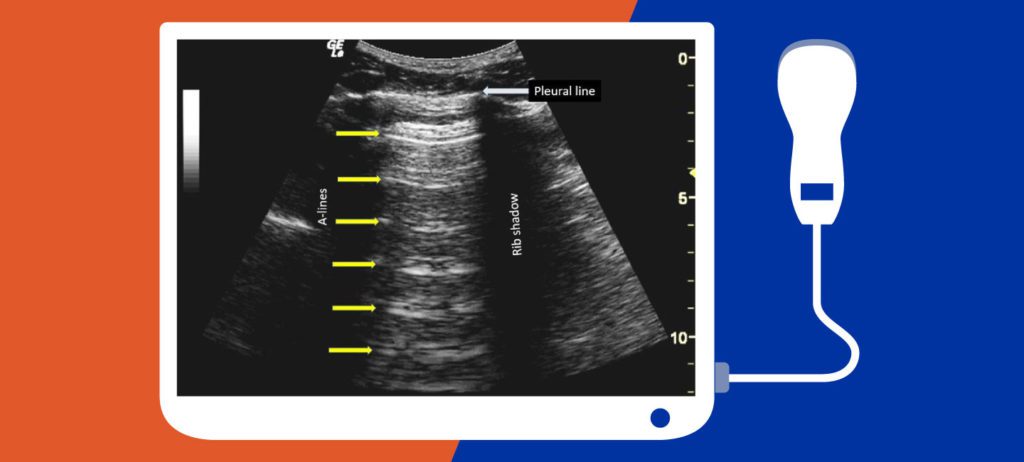
The recommended transducer for chest ultrasound is dependent on how deep you wish to image in the chest and how much resolution is required. The ideal goal is to obtain the best possible images with the highest possible resolution. For example, if the goal is to image the pleura and observe lung sliding, then a high-frequency linear transducer is the best choice. If the goal is to observe A-lines or B-lines, then a low-frequency curvilinear transducer (2.0 – 4.5 MHz) would be ideal. In the modern single probe devices, you need to select the “Lung or Chest” preset to optimize it for the best results.
From superficial to deep, you will see epidermis, dermis, connective tissue, adipose tissue layer, ribs and intercostal muscles, parietal and visceral pleura, and the pleura lung interface. Lung/pleural sliding is seen better with a high-frequency linear transducer (10.0 – 12 MHz range or higher). The significant change in acoustic impedance at the pleura – aerated lung interface results in horizontal artifacts that fade into the distance and are equidistant from each other (see figure above). Therefore, it is essential to set the optimal depth of 15 cm or more and use a low-frequency curvilinear transducer.
The rib’s anterior cortical layer is highly reflective, and so it will be seen as an echogenic line with a posterior acoustic shadow deeper into it. If you are scanning closer to the midline, then the cartilage will appear as an anechoic space without any posterior acoustic shadowing.
The best feature of lung ultrasound is that it is easy to perform, and it allows you to monitor the patient’s progress with no added risk of exposing the patient to unnecessary ionizing radiation. This form of imaging is beneficial, especially in the pediatric patient population. Also, it is very sensitive and specific to detect free pleural effusion as compared to standard chest X-ray views.
The figure shows a normal lung ultrasound view obtained by placing the transducer in the longitudinal plane with the probe marker pointing cephalad. Observe the A-lines (yellow arrows) and the rib shadows. Note that the A-lines are equidistant and fade away into the distance. A-lines alone only suggest the presence of air in the chest region.
Looking for additional inspiration? Sign up for our POCUS Post™ newsletter to receive monthly tips and ideas.