Victor V Rao MBBS, DMRD, RDMS (APCA)
The abdominal aorta is the largest artery in the abdominal cavity and is a continuation of the thoracic aorta. As seen in Figure 1 below, it runs almost parallel to the inferior vena cava (IVC) and is located just anterior to the lumbar vertebral bodies and intervertebral disc spaces. It follows the curvature of the lumbar vertebral column because of its location just anterior to the lumbar spine. It divides at the level of the umbilicus into the right and left common iliac arteries.
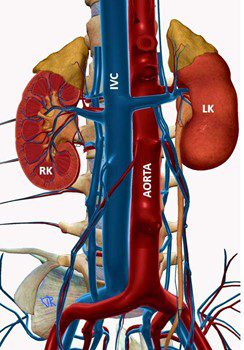
Fig. 1 Abdominal aorta and IVC.
An abdominal aortic aneurysm (AAA) is a dilatation of the abdominal aorta with a diameter of 3.0 cm or more. The average normal infrarenal aorta diameter is approximately 2.0 cm. If the aorta is dilated and the maximum diameter is less than 3.0 cm, it is called aortic ectasia. An abdominal aortic aneurysm could be classified as either a fusiform or berry aneurysm based on its morphology.
AAA occurs due to weakening in the wall of the abdominal aorta. The high pressure within the lumen of the abdominal aorta further weakens the wall segment causing it to balloon out like a worn radiator or garden hose. The weakened wall may rupture or leak when all three layers of the artery are disrupted. Sometimes, the inner layer is disrupted, and the blood enters the space between the inner and middle layers. If the blood continues to spread, it produces a condition known as aortic dissection.

Fig. 2 Fusiform dilatation of a radiator hose due to weakening of the wall over time. A fusiform abdominal aortic aneurysm looks very similar in appearance.
According to the Centers for Disease Control and Prevention, 9,904 deaths were reported in the US due to aortic aneurysm rupture or aortic dissection in 2019. Mortality rates due to AAA rupture range from 32% to 70%, with very high morbidity even with significant advances in medical care. Fifty-nine percent of the patients who died due to AAA rupture were men. It is interesting to note that 75% of all patients diagnosed with AAA have a history of smoking. Due to this strong association, the United States Preventive Services Task Force (USPSTF) recommends a one-time screening for AAA in men aged 65-75 with a smoking history. An individual who has stopped smoking but had been smoking in the past would also qualify.
AAA may develop at a much earlier age in patients with connective tissue disorders such as Marfan syndrome. These individuals may require AAA screening when younger. Since the mortality rate in patients with a ruptured AAA is very high, it is advisable to screen patients and diagnose the condition early. Regular follow-up and/or providing corrective intervention options before the aneurysm ruptures are also imperative.
Patients with AAA could be asymptomatic or could present with a pulsatile abdominal mass, vague abdominal, back or groin pain, or may even present with hypovolemic shock if the abdominal aortic aneurysm has ruptured. The ideal transducer for performing a AAA screen is a low-frequency curvilinear transducer. Use the abdomen preset and a depth setting of 15 – 20 cm. The depth and gain should be adjusted to obtain the best image possible. The spine and associated spine shadow are useful landmarks and should be visible in the image. Bowel gas could obstruct the view due to the dirty gas shadow produced by the bowel gas. Gentle pressure with the transducer or slightly sliding the probe can help obtain a clear image of the aorta.
Small abdominal aortic aneurysms ranging from 3.0 – 5.5 cm are generally managed by routine follow-up rather than surgical correction due to the risks associated with open surgery. Endovascular stent placement is another treatment option with a lower risk of mortality and a quick recovery time.
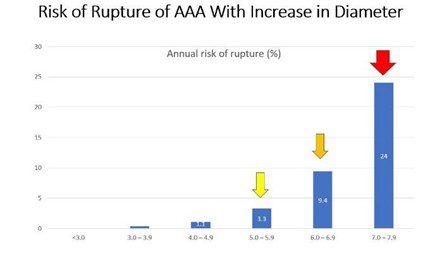
Fig. 3 Graph showing the risk of rupture of an aortic aneurysm with the increase in the maximum diameter of the aneurysm. The risk increases almost three times when the diameter is 6.0 – 6.9 cm and then more than doubles again once it reaches 7.0 cm or more.
Even though the risk of aneurysm ruptures increases significantly with an increase in diameter, we rarely encounter patients with very large aortic aneurysms that have not ruptured. One of the largest abdominal aortic aneurysms reported in literature was 25.0 cm in diameter. This was a rare case as most aneurysms of the abdominal aorta tend to leak or rupture when the diameter increases beyond 5.5 cm. The patient described in the article underwent open surgical repair with a remarkable outcome, living for seven years post-surgery. See reference article 1.
An abdominal aortic aneurysm can be diagnosed using ultrasound very effectively, particularly when the entire length of the abdominal aorta is visible on ultrasound. Sensitivity and specificity of the ED US were reported to be 99% and 98% by Elizabeth Rubano et al. During the AAA ultrasound screen examination; views should be obtained at the upper, mid, and lower abdominal aorta in both the transverse and mid-longitudinal planes. Each view should be labeled with a measurement of the maximum diameter of the abdominal aorta. If an aneurysm is detected, then always capture additional views, and record the site of the aneurysm. Labeling, measuring, and documenting properly for follow-up studies is vital.
If the aneurysm is not large enough for intervention, then serial follow-up exams are recommended depending on the maximum diameter of the aneurysm. All aneurysms tend to increase in diameter over time. Bowel gas and obesity may pose some challenges. Use a curvilinear low-frequency transducer and adjust the depth setting to the maximum possible during scanning. If a curvilinear transducer is unavailable, you can use a low-frequency phased array transducer.
The depth must be adjusted to optimize the image since the upper abdominal aorta is much further away from the anterior abdominal wall than the lower abdominal aorta. Once the abdominal aorta and the spine posterior to it are identified, adjust the depth to obtain an optimal image. Measure the true maximum diameter from outer wall to outer wall. A tortuous abdominal aorta may be very challenging to measure accurately.
If an aneurysm is present, measure the maximum diameter in both the mid-longitudinal and transverse planes from the outer wall to the outer wall. If a thrombus is present within the aneurysm, include the thrombus in the measurement. A potential pitfall could be accidentally measuring the oblique diameter and overestimating it. It is important to measure accurately as the management depends on the maximum diameter of the aortic aneurysm.
In conclusion, there is hope that with the global adoption of point-of-care ultrasound, more AAA cases will be detected early—before they rupture or dissect. This increased adoption may further reduce mortality rates due to ruptured abdominal aortic aneurysms.
Start your POCUS Abdominal Aortic Aneurysm Certificate here.
References





















