By Victor Rao MBBS, DMRD, RDMS
Introduction
Lung ultrasound (LUS) has emerged as one of the most important diagnostic imaging tools in modern medicine. This blog article explores its historical evolution, scientific principles, and current clinical relevance based on peer-reviewed research and modern applications in point-of-care ultrasound (POCUS). Every clinician should learn to perform lung ultrasound and implement it in patient care when indicated.
Historical Perspective
The piezoelectric effect was first discovered in 1880 by the French physicist brothers Pierre Curie and Jacques Curie. Their research demonstrated that applying mechanical pressure to certain crystals, such as quartz, produces an electric charge on the crystal surface. After the Titanic disaster in 1912, there was a significant push to create underwater detection systems capable of finding icebergs. Canadian engineer Reginald Fessenden built the first working sonar system in 1914, primarily to detect icebergs. His sonar device could identify an iceberg underwater from 2 miles away.
Paul Langevin played a key role during World War I by inventing the first practical ultrasonic submarine detector, which became the foundation for sonar technology. Initially developed for submarine detection during World War I, its medical potential was realized in 1937, when Karl and Friedrich Dussik first used ultrasound for neuroimaging. The integration of ultrasound into medical diagnostics took off through the 1950s and 1960s, revolutionizing obstetrics, cardiology, and internal medicine.
In 1987, Dr. Norman Rantanen, a pioneering equine veterinarian, was the first to apply lung ultrasound in veterinary medicine for diagnosing pneumothorax in horses. This marked the first documented veterinary use of lung ultrasound. Within a year, similar findings were published in human medicine. However, lung imaging lagged because air scatters sound waves, producing artifacts instead of structural images of normal lung tissue.
This changed in the late 1990s when French intensivist Daniel Lichtenstein recognized that these artifacts which were once seen as limitations carried valuable diagnostic information about lung pathologies. His pioneering work, notably the description of B-lines (comet-tail artifacts) in 1997, led to a new interpretive model for lung ultrasound.
Physical and Imaging Principles
Lung ultrasound works by sending ultrasound waves into the chest. Since normal healthy lung tissue is filled with air, it reflects most of the ultrasound signal, creating characteristic artifacts rather than direct anatomical images. These artifacts, once considered limitations, are now recognized as valuable diagnostic clues. The key ultrasound signs include the following:
- A-lines: Horizontal, evenly spaced lines that indicate normal, air-filled lungs.
- B-lines: Vertical artifacts that arise from the pleura and suggest fluid in the lung, such as in interstitial or alveolar edema.
- Seashore sign (M-mode): A wavy pattern that reflects normal pleural movement.
- Stratosphere sign: A barcode-like pattern indicating absent pleural sliding, consistent with pneumothorax. You can artificially create this in a normal patient by asking the patient to stop breathing.
Below are some ultrasound images which every POCUS user should be familiar with.
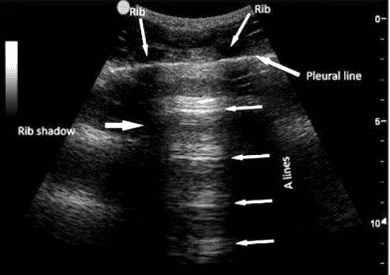
Figure 1. Normal lung (A-lines): Parallel, equidistant, horizontal lines below pleural line. Note the location of the pleural line, ribs, rib shadows. Observe how the A-lines tend to fade away (less echogenic and even less clear) as they appear further away from the transducer footprint. In contrast, B-lines extend to the bottom of the screen without fading or losing intensity (See Figure 2).
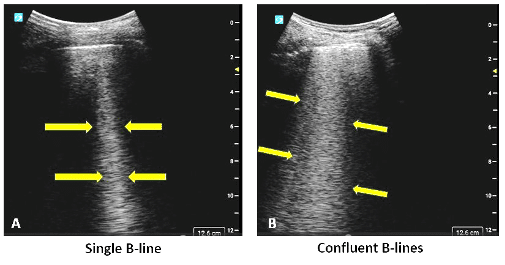
Figure 2. (A) A single (B-line) vertical hyperechoic artifact arising from pleural line and extending to the bottom of the screen away from the transducer footprint without fading in intensity. To demonstrate B-lines set the depth to approximately 12-15 cm. Image on the right (B) shows multiple confluent B-lines.
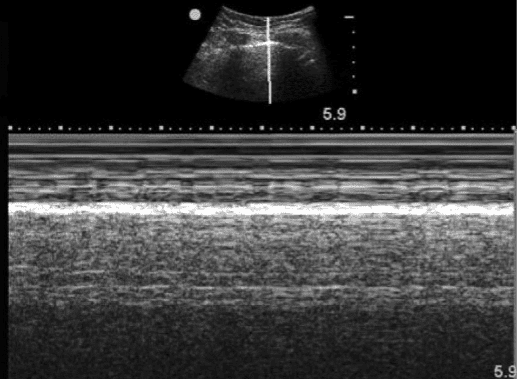
Figure 3. Seashore sign on M-mode.
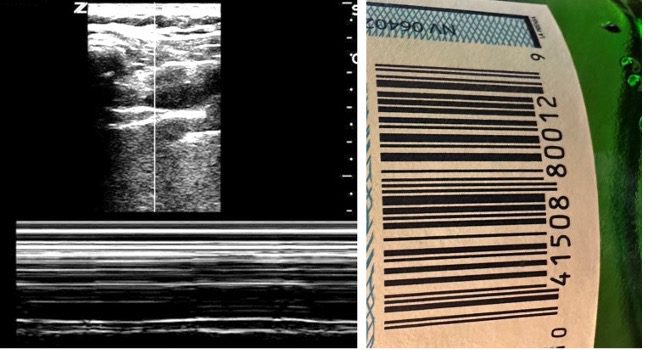
Figure 4. Pneumothorax – Stratosphere sign or Barcode sign (M-mode). Observe that the barcode sign on the left is very similar to the barcode on a product (right).
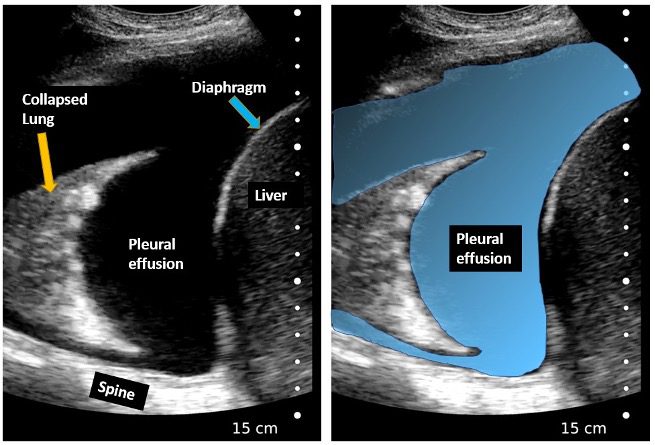
Figure 5. Right pleural effusion. Spine is seen superior to the diaphragm (Spine sign positive), Large anechoic pleural effusion seen. Right lung is collapsed (atelectasis).
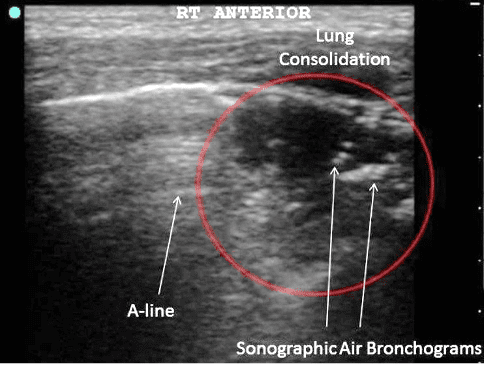
Figure 6. Bacterial pneumonia – small lung consolidation with air bronchograms. Courtesy Springeropen.com (see link in references)
The BLUE (Bedside Lung Ultrasound in Emergency) protocol, published by Lichtenstein in 2008, standardized LUS application, making it invaluable in diagnosing conditions such as pneumothorax, pulmonary edema, pneumonia, and ARDS within minutes using portable ultrasound equipment.
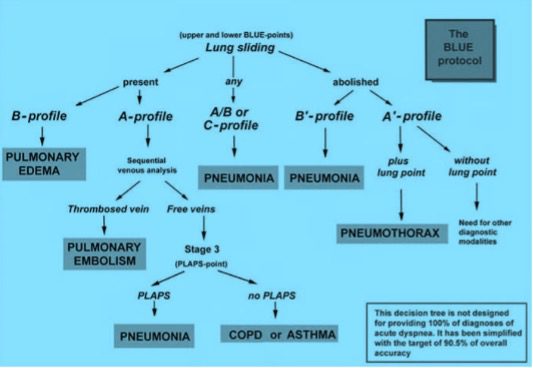
Figure 7. BLUE Protocol. Courtesy Chest 2008; 134:117-125.
Diagnostic Applications and Evidence
Extensive peer-reviewed research shows that lung ultrasound (LUS) is effective in diagnosing a range of pulmonary conditions and often outperforming chest X-rays and approaching the accuracy of CT scans.
- Pneumonia: Lung ultrasound can detect lung consolidations with over 95% specificity. These appear as subpleural hypoechoic zones with dynamic air bronchograms, making lung ultrasound a reliable tool for diagnosing pneumonia.
- Pleural Effusion: Lung ultrasound is sensitive enough to identify even small effusions that may be missed on radiographs. Studies by Roch et al. (2005) and Yang et al. (1992) confirm its high diagnostic accuracy.
- Pulmonary Edema: The presence and distribution of B-lines on ultrasound correlate with extravascular lung fluid, offering a non-invasive way to assess fluid overload and congestive status.
- Pneumothorax: The absence of lung sliding and the presence of a “lung point” on ultrasound is pathognomonic for pneumothorax. LUS is often more reliable than supine chest X-rays in detecting a small pneumothorax.
In 2012, the International Consensus Conference on Lung Ultrasound (ICC-LUS) established global guidelines for terminology, protocols, and training. These recommendations emphasized lung ultrasounds utility across critical care, anesthesia, and cardiology, and called for standardization to ensure consistent and reproducible results.
Technological Advancements and AI Integration
In recent years, the development of handheld ultrasound devices has significantly expanded access to lung imaging. These portable tools are cost-effective, easy to use, and ideal for bedside assessments in emergency departments, outpatient clinics, and in resource-limited settings.
A major innovation in this space is the integration of artificial intelligence (AI). AI-powered software can automatically detect key ultrasound patterns, such as pleural line abnormalities and B-line density, offering real-time diagnostic support. This is especially valuable for clinicians with limited ultrasound experience, as it enhances accuracy and consistency.
Studies like those by De Rosa et al. (2022) and platforms such as Deep Breathe AI demonstrate how machine learning algorithms can assist in interpreting lung ultrasound images. These tools help streamline workflows, reduce diagnostic errors, and support clinical decision-making.
Summary and Future Outlook
Lung ultrasound has progressed from its early military applications to become an essential modality for point of care lung evaluation. Initially considered “not possible” due to limitations posed by normal aerated lung tissue, it is now recognized for its diagnostic accuracy, portability and absence of ionizing radiation, making it an important modality in healthcare and specifically in critical care, emergency medicine, pediatrics, primary care and resource-limited settings.
Ongoing research aims to refine quantitative scoring systems (e.g., Lung Ultrasound Score) and integrate LUS into remote telemedicine frameworks, ensuring continued democratization of access to advanced pulmonary diagnostic tools worldwide. Lung ultrasound is a relatively easy skill to learn with a short learning curve. Every clinician should strongly consider learning this skill to better serve their patient population.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3734893/
- https://link.springer.com/article/10.1007/s00134-012-2513-4
- https://www.atsjournals.org/doi/10.1164/ajrccm.156.5.96-07096
- https://www.deepbreathe.ai/blog/lung-ultrasound-a-brief-history
- https://www.sciencedirect.com/science/article/abs/pii/S0012369215323977
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9388019/
- https://www.wendyblount.com/articles/ultrasound/2Article-LungUS-2015IVECCS-Lisciandro.pdf
- https://theultrasoundjournal.springeropen.com/articles/10.1186/2036-7902-4-16




















