By Victor Rao MBBS, DMRD, RDMS
Introduction
Haglund’s deformity is an abnormal bony enlargement at the posterosuperior aspect of the calcaneus, where the Achilles tendon is attached. This bump can be easily seen (See Figure 1) and palpable during a physical examination.
I am sure we have all observed this condition in our patient population. This deformity was first described by a Swedish orthopedic surgeon Patrick Haglund in 1927. This condition is also known as retrocalcaneal exostosis, Mulholland deformity, and “pump bump”. The bony bump can cause irritation of the distal Achilles tendon and adjacent bursae.
The Achilles tendon forms from the gastrocnemius and soleus muscles, inserting onto the posterior calcaneus. It is important to note that Haglund’s deformity can lead to Haglund’s syndrome and not all patient’s with Haglund’s deformity have Haglund’s syndrome. Haglund’s syndrome refers to a triad of Haglund’s deformity, retrocalcaneal bursitis and insertional Achilles tendinopathy.
The retrocalcaneal bursa (between the Achilles tendon and calcaneus) and the superficial subcutaneous bursa (between the skin and the Achilles tendon) are commonly associated with the inflammation seen in patients with symptomatic Haglund’s deformity. This deformity can cause discomfort when wearing certain types of shoes such as work boots, dress shoes, ice skates etc.
The exact cause is not fully understood. Some factors such as high arch, genetics, tight Achilles tendon, foot mechanics (poor gait pattern) or shoes with rigid backs could be a contributing factor. Even though the exact epidemiological incidence data is limited, a best estimate is that approximately 2% of the population may be affected, more commonly in the middle age group with a higher female predominance. However, among patients with insertional Achilles tendonitis, the rate of Haglund’s syndrome has been reported to be up to 25%.
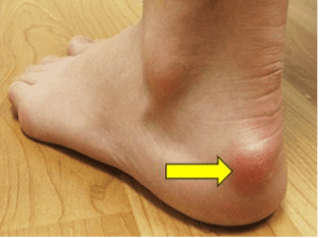
Figure 1. Haglund’s deformity (yellow arrow). A visible bump is seen on the back of the heel.
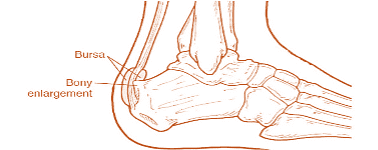
Figure 2. Diagrammatic representation of Haglund’s deformity. Observe the abnormal bony enlargement on the posterosuperior aspect of the calcaneal tuberosity and how it is affecting the Achilles tendon and the adjacent bursae.

Figure 3. Plain X-ray shows a prominent bony prominence on the posterosuperior aspect of calcaneal tuberosity. Slight convexity of the soft tissue is observed at the site of Achilles tendon. The vertical distance value >4 mm from the bump to the reference line on the posterior aspect of the calcaneus suggests Haglund’s deformity.
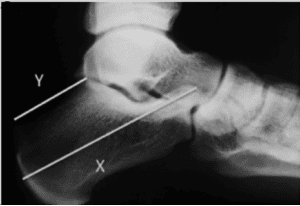
Figure 4. Calcaneus measurements in Haglund’s syndrome. Note that X:Y ratio is less than 2.5. Image courtesy of Yves Tourné et al. See reference article.
Anatomical Review
The Achilles tendon connects the calf muscles namely gastrocnemius and soleus to the calcaneus (heel bone). It is the thickest and strongest tendon in the human body. It is a critical structure for certain movements such as walking, running and jumping and helps to push off the ground by enabling plantar flexion of the foot and transmitting the power of the calf muscles to the foot. It is approximately 6-10 inches long for an average adult.
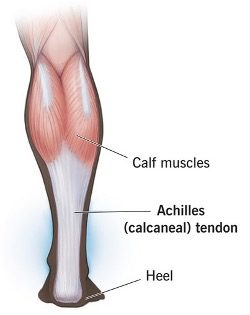
Figure 5. Achilles tendon (diagrammatic representation). Image courtesy of Cleveland Clinic
Ultrasound Technique Tips
Patient Position
Prone, foot hanging free, allowing dynamic ultrasound assessment.
Transducer
High-frequency linear transducer with a frequency range of 10–15 MHz is ideal for optimal imaging of this condition.
Scan Planes
Long-axis – Parallel to Achilles tendon fibers.
Short axis – Perpendicular to tendon for displaying cross-sectional anatomy.
Dynamic Maneuvers
Passive dorsiflexion/plantarflexion to visualize tendon gliding and bursa distension.
Doppler
Power Doppler or color Doppler are helpful to document hyperemia within the tendon or around the bursae, suggestive of active inflammation. Note that power Doppler is a more sensitive modality to detect hyperemia.
Sonographic Findings in Haglund’s Deformity
- Posterosuperior calcaneal exostosis (the “bump”).
- May see underlying calcaneal spur.
- Focal thickening at the insertion (normal: 4–6 mm; >7–9 mm or more suggests pathology).
- Loss of normal fibrillar echotexture—appears hypoechoic and swollen.
- Insertional tendinopathy and/or partial thickness tears.
- Hyperemia on Doppler in chronic/active inflammation.
- Retrocalcaneal bursa: Anechoic or hypoechoic distension (fluid collection).
- Superficial/subcutaneous bursa: Hypoechoic swelling between skin and tendon. Both structures may appear enlarged and inflamed.
- Convexity of soft tissues posterior to the tendon (superficial bursitis).
- Disrupted interface where tendon meets calcaneus.
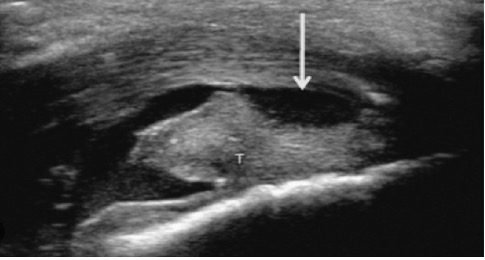
Figure 6. Retrocalcaneal and Achilles bursitis. Image courtesy of Radiology Key
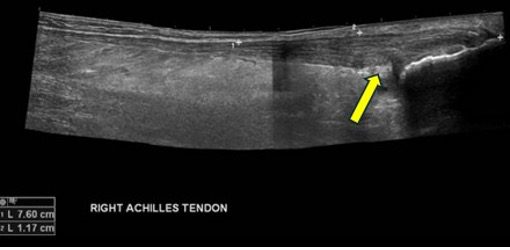
Figure 7. Distal swelling of Achilles tendon. Kager’s fat pad appears echogenic (arrow). Image courtesy of Radiopedia.org
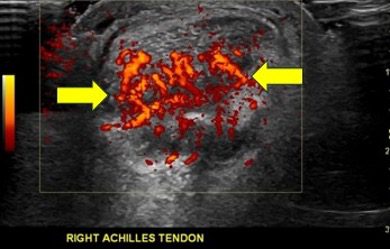
Figure 8. Hyperemia of Achilles tendon, fat pad and bursa on power Doppler. Image courtesy of Radiopedia.org
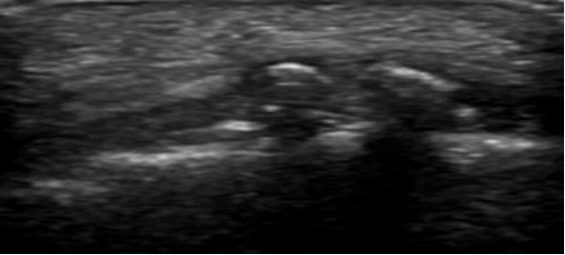
Figure 9. Retrocalcaneal bursitis. Image courtesy of Radiopedia.org
Advantages of Using POCUS
POCUS offers unique advantages to clinicians in this condition such as:
- No exposure to ionizing radiation.
- Real-time dynamic assessment.
- Soft-tissue differentiation—can distinguish tendinopathy, tears, and bursitis.
- Guidance for procedures—injection of corticosteroids into bursa under direct visualization.
- Cost-effective and easily accessible compared to MRI.
- Excellent tool for monitoring healing over time.
Differential Diagnosis
Plain radiographs and MRI can confirm bony abnormalities, but correlation with sonographic soft tissue detail supports the diagnosis. Other causes of heel pain include isolated retrocalcaneal/superficial bursitis, systemic arthropathies, and Achilles tendon tear.
Conclusion
Ultrasound is a highly effective modality for evaluating or diagnosing Haglund’s deformity, and Haglund’s syndrome and helps define both bony and soft-tissue pathology surrounding the Achilles insertion. Key findings include a posterosuperior calcaneal bump, thickened and hypoechoic tendon, retrocalcaneal and superficial bursitis, and increased Doppler flow in active inflammation.
POCUS assessment protocol involves assessing the tendon and adjacent tissues in multiple planes, including dynamic assessment and color or power Doppler imaging. Treatment options include shoe modification, stretching exercises, anti-inflammatory medication, ice application, and physical therapy. Surgery is rarely recommended and reserved for unresponsive cases to remove the bony prominence. The goal of this blog article is to helps POCUS users confidently diagnose Haglund’s deformity and Haglund’s syndrome.
References
- Sofka et al, Haglund’s Syndrome: Diagnosis and Treatment Using Sonography, HSS J. 2006 Feb;2(1):27–29. doi: 10.1007/s11420-005-0129-8
- https://radiopaedia.org/articles/haglund-syndrome?lang=us
- International Journal of Sports Physical Therapy, Diagnostic Musculoskeletal Ultrasound of the Achilles Tendon (2025) https://pubmed.ncbi.nlm.nih.gov/39906049/
- Haglund’s Deformity and Chronic Achilles Tendonitis Charles L. Myerson BA et al. doi: 10.1053/j.oto.2018.02.006
- Contribution of a new radiologic calcaneal measurement to the treatment decision tree in Haglund syndrome Yves Tourné et al. doi: 10.1016/j.otsr.2018.08.014
Additional Content (YouTube Video by Niek Vink)




















