By Victor Rao MBBS, DMRD, RDMS
Introduction
The extended Focused Assessment with Sonography for Trauma (eFAST) is an ultrasound protocol for a quick evaluation of trauma patients with suspected occult abdominal and thoracic injuries. It is designed to identify life-threatening conditions such as hemoperitoneum, hemothorax, pneumothorax, hemopericardium and cardiac tamponade. It is a low-cost practical tool in mass trauma situations as an excellent triage tool.
Be aware that the value is in a positive examination. A negative study could indicate that there is no internal injury, or the amount of internal bleeding is not significant enough to be diagnosed by ultrasound at that point in time. If there is a high index of suspicion of internal injury with a negative eFAST examination and if the patient is hemodynamically stable, CT scan should be considered. If CT scan is not available, then serial ultrasounds must be performed along with monitoring on patients’ vital signs as per recommended protocol.
Indications
There are several indications for performing an eFAST examination. The common indications are:
- Hemodynamically unstable patients with H/O blunt abdominal or chest trauma.
- Hemodynamically stable patients with H/O blunt abdominal or chest trauma.
- Patients with penetrating injury to the chest or abdomen.
- Trauma patients with acute clinical deterioration suggesting internal bleed.
eFAST Protocol
The eFAST examination consists of five main ultrasound views. They are:
- Right Upper Quadrant (RUQ): Examine for free fluid in the hepatorenal (Morison’s pouch) and right lower thoracic cavity. Also examine the region around the inferior edge of the right lobe of the liver and beyond. Free fluid may appear first around the tip of the right lobe of the liver before being detected in the Morison’s pouch.
- Left Upper Quadrant (LUQ): Examine for free fluid in the splenorenal recess (Koller’s pouch), around entire perimeter of the spleen and left thoracic cavity.
- Subxiphoid (Pericardial sac): Examine for pericardial effusion and cardiac tamponade. Tamponade is life threatening condition and must be addressed immediately.
- Pelvic (Suprapubic): Assess for free fluid in the rectovesical pouch in males or cul-de-sac/ pouch of Douglas in females.
- Bilateral Anterior Chest: Assess for pneumothorax.
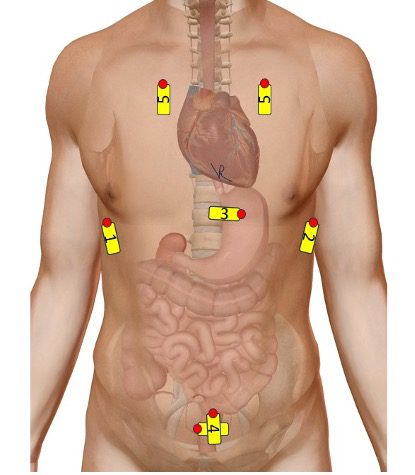
Figure 1. Diagrammatic representation of locations of transducer placement and transducer image orientation marker direction for the eFAST views. The red dots indicate the transducer image orientation marker. For example, transducer position 1, the transducer orientation marker is pointing cephalad.
Procedure – General Guidelines
The patient should be in a supine position. Use a curvilinear transducer for optimal ultrasound beam penetration. Some clinicians also consider using a low frequency phased array transducer. Systematically scan each of the five regions, looking for anechoic (black) areas indicating free fluid as well as ultrasound findings suggestive of pneumothorax. If an optimal cardiac view is not available in the subxiphoid region, you can opt to obtain a left parasternal long axis (PLAX) view of the heart. The examination can be completed in under two minutes by an experienced clinician.
Interpretation and Clinical Application
Positive eFAST
Detection of free fluid in the peritoneal cavity or pneumothorax/hemothorax is highly suggestive of significant injury and may require immediate surgical or procedural intervention, especially in hemodynamically unstable patients.
Negative eFAST
A negative result does not completely rule out internal injury, especially early after trauma or in cases of hollow organ injury, as sensitivity is lower when there is minimal or no free fluid. Serial eFAST examinations may be necessary in patients with negative eFAST and a high clinical suspicion or evolving symptoms such as tachycardia, dyspnea and lowering serial blood pressure.
eFAST Diagnostic Accuracy and Limitations
| Clinical Condition | Sensitivity | Specificity | Additional Comments |
| Free fluid in the abdominal cavity | 69-91% | 99% | Higher sensitivity when larger volume of free fluid is present |
| Pneumothorax | 87% | 98% | More sensitive than Chest X-ray |
| Hemothorax | 99.5-100% | 100% | |
| Cardiac tamponade | 98.2% | 98.5% |
Table 1. Sensitivity and specificity of eFAST examination components. Do note that sensitivity and specificity vary by different authors/researchers due to a variety of reasons.
Limitations
Reduced sensitivity for hollow viscus or mesenteric injuries without free fluid. Air in the peritoneal or pleural space (e.g., from penetrating trauma) can obscure views. Obesity, subcutaneous emphysema, and operator experience can affect image quality.
Which Patients May Benefit Most From an eFAST Examination
eFAST is most valuable in unstable trauma patients who cannot be safely transported from the emergency department for a CT scan. A positive eFAST can expedite definitive care (e.g., surgery, chest tube placement) without delay. In stable patients or those with negative eFAST but ongoing suspicion, further imaging (CT) or serial ultrasound may be warranted. eFAST is a non-invasive, repeatable, and rapid diagnostic tool that improves trauma care efficiency and outcomes without exposing the patient to unnecessary harmful ionizing radiation.
eFAST Views and Findings (Diagnostic Findings and Key Landmarks)
| View | Diagnostic Finding | Important Anatomical Landmarks |
| Right Upper Quadrant (RUQ) | Hemoperitoneum, hemothorax | Right lobe of liver, right hemidiaphragm to include right costovertebral angle, Morison’s pouch |
| Left Upper Quadrant (LUQ) – may be a little bit more difficult view to obtain | Hemoperitoneum, hemothorax | Spleen, splenorenal recess (Koller’s pouch), all around the spleen and left hemidiaphragm to include left costovertebral angle |
| Subxiphoid view | Pericardial effusion/ cardiac tamponade | Heart, pericardium, pericardial sac, diaphragm, liver |
| Pelvic cavity | Hemoperitoneum | Bladder, rectovesical pouch in males and cul-de-sac in females |
| Anterior Chest (Bilateral) | Pneumothorax | Pleural line, lung sliding |
Table 2. eFAST views with important landmarks to be included in the views and diagnostic positive finding.
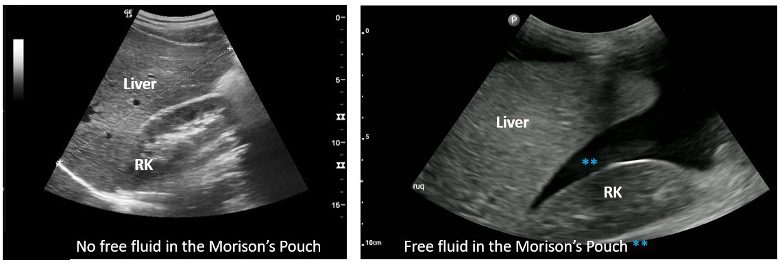
Figure 2. The image on the left shows a normal Right Upper Quadrant (RUQ) view with no evidence of fluid in the Morison’s pouch. The image on the right shows anechoic free fluid ** present in the Morison’s pouch.
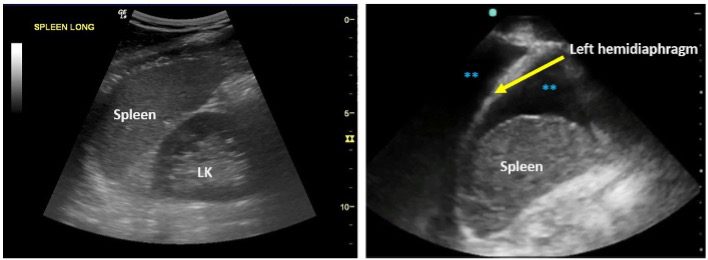
Figure 3. The image on the left shows a normal Left Upper Quadrant (LUQ) with no evidence of free fluid in the perisplenic region and the left costovertebral region. The image on the right shows evidence of anechoic free fluid ** seen between the spleen and the left hemidiaphragm. Note the echogenic left hemidiaphragm. Anechoic free fluid ** is also seen above the left hemidiaphragm in the left chest cavity. This was a case of hemothorax and hemoperitoneum secondary to trauma.
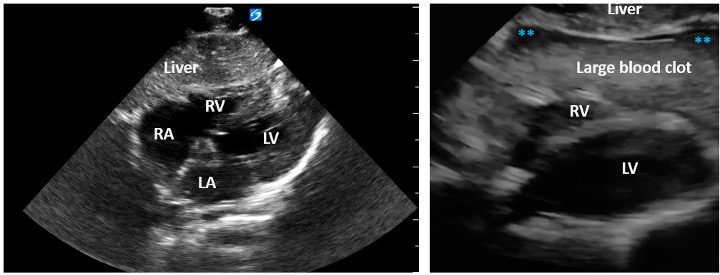
Figure 4. Subcostal/subxiphoid view of the heart on the left with no evidence of fluid in the pericardial sac. The image on the right shows RV is compressed due to a large pericardial effusion. A large echogenic thrombus is seen in the pericardial with small amount of anechoic unclotted blood **. This lesion could easily be missed. The blood clot was more easily detectable on live B-mode imaging. Always look carefully. The patient is in cardiac tamponade, which is a life-threatening condition and must be treated immediately to avoid serious complications or mortality.
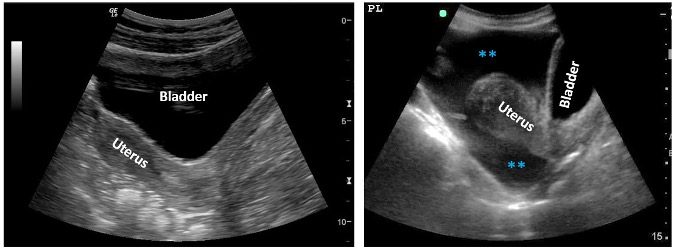
Figure 5. The image on the left shows a mid-sagittal view of the female pelvic region. Observe the location of the uterus and the bladder anterior to it. The image on the right shows a similar view but with evidence of free fluid ** in the pelvic cavity and the pouch of Douglas/cul de sac. Observe the location of the bladder.
The eFAST assessment for pneumothorax consists of views obtained in both upper anterior chest to look for evidence or absence of lung sliding. Normally, lung sliding should be seen when the patient is breathing. If lung sliding is absent, then try to locate the lung point as well as perform an M-mode tracing. Normally, in an aerated lung the seashore sign is seen. In case of pneumothorax the barcode or stratosphere sign is seen.
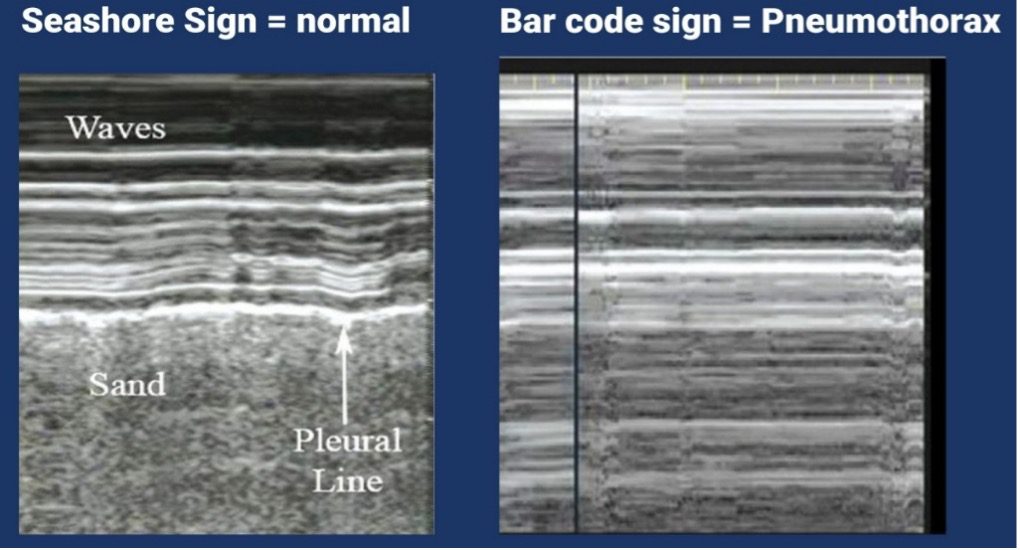
Figure 6. The image on the left shows a normal seashore sign. The image on the right shows a barcode sign which is suggestive of a pneumothorax. In addition, look for absent lung sliding and lung point.
Final Thoughts
The original FAST examination has evolved into the eFAST examination. And is considered an essential tool in 21st century trauma evaluation, allowing for the rapid identification of life-threatening occult bleeding and pneumothorax at the point of care. While highly specific, its sensitivity is greatest when detectable levels of free fluid are present. Good clinical judgment and repeat assessments remain crucial especially if the eFAST examination is negative.
Ultrasound may not be very sensitive for diagnosing solid organ injury as compared to CT scan. The real value of the eFAST examination is in a positive examination finding. Be aware that a negative eFAST could suggest that either there is no internal bleed or the amount to internal blood loss has not yet reached the detectable levels with ultrasound. Even though most of the time, the free fluid/blood will appear anechoic, it is important to be aware that sometimes blood may appear hyperechoic. Always try to correlate clinically to avoid potential pitfalls. Do not confuse yourself with ascites or renal cysts. The goal of this blog article is to inspire all clinicians to learn this easy to master lifesaving ultrasound skill and familiarize everyone with normal and abnormal findings.
References




















